Posted: Sat Apr 16, 2011 1:46 pm
Dr. Sclafani,
Do you treat CCSVI in a hospital in New York? or only in the clinic?
thanks
Pam
Do you treat CCSVI in a hospital in New York? or only in the clinic?
thanks
Pam
Welcome to This is MS, the leading forum for Multiple Sclerosis research and support. Join our friendly community of patients, caregivers, and researchers celebrating over 20 years of delivering hope through knowledge.
https://www.thisisms.com/forum/
civickiller wrote:Dr. Sclafani,
I believe stenosis is caused from something(bone or muscle) putting pressure on the vein. Have you seen stenosis at one section of the vein but when you went back in a 2nd time, seen stenosis at a different position of the same vein? why is it that almost every MR scan ive seen shows either a pinched vein or looks like the vein is getting pressured to close, from only 1 side of the vein?
Thanks

You are indeed fortunate that your thrombosis was able to reverse itself while on coumadin. Often, occlusion of the jugular vein is a permanent thing. You might not have had such an outcome if this vein had been the second vein treated rather than the first one.CD wrote:Hi Dr. Sclafani,davmets2 wrote:Dr Sclafani,
I just had my 3 month ultrasound. My procedure was done in 2 stages, one week apart. While doing the second procedure for the RJV the venogram showed that the LJV that was done the week before with 18 mm balloon had restenosed and clotted. He attempted to re-balloon without any success. Had been on warifin since then (just stopped taking yesterday).
The ultrasound that I just had done yesterday showed flow in both jugulars. He couldn't tell me how much flow. He suggested another procedure with ballooning and probably a stent, but gave no guarantees that this would work or help. He told me to think about it, but the sooner I do it the better chances of success.
I guess my question would be, is there any test to show how much flow I'm getting and do you think that I should consider another procedure, possibly with a different Dr. such as yourself.
Thanks
I thought this was a good question. I, too, would be interested in your opinion on this question, whenever you have the time to answer. I know you are a very busy doctor.
Thanks,
CD
I have done about 100 cases at American Access Care in an ambulatory setting co-working with nephrologists/intensivists who perform interventions on renal dialysis fistulas and grafts for patients in chronic renal failure. One patient has required a two day admission for congestive heart failure. This is pretty satisfactory, considering I will treat patients despite high EDDS. I think admission to the hospital is really overutilizing the health care system for the most part. Come patients may need admission prior to the procedure, but these are rare.pklittle wrote:Dr. Sclafani,
Do you treat CCSVI in a hospital in New York? or only in the clinic?
thanks
Pam
Firstly:drsclafani wrote:firstly, we must ask what was the intention behind the first intervention. Was it to eliminate some painful symptoms? to reverse some weakness or sensory mprove balance? to reverse fatigue ?vivavie wrote:If my stents are occluded what are my options, I am already on coumadin and plavix? I have a stent within stents within stents (3 layers), Is there anything more that can be done? should I even bother to get that US?
the ask whether that accomplished that. that is the first piece of the puzzle.
Secondly, if you had reversal of fortunte and symptoms returned, then was the original improvement of great value or a minor disappointing improvement.
Thirdly, what was the purpose of putting the first stent in? was it a regretful treatment plan or did it provide you with some worthwhile improvement
Fourthly, we know what the purpose of putting the last stents in. Did it provide what you were looking for.
After answering these questions, we can have a meaningful discussion of how much further to pursue this. Only you can answer these questions.
But, you are in pain, we do not know why. treatment, no treatment, i think it is important to understand what is going on because we cannot have a logical discussion with out knowing that.
drs
So if an ant is small, should Aunt Bertha be a diminutive 325 pounds?bluesky63 wrote:That last post was at 1:20 a.m. The doctor that never sleeps!
I hope I say this right, but I was just reading your response to Lyme Nurse about how the MRV can be inaccurate. And I know my MRV was not accurate compared to my venogram. So if MRVs can be so off, what about MRIs? I know this isn't your field, but doctors rely so much on MRIs. And all MS patients (and the best MS doctors) know from experience that the MRI does not necessarily match the clinical picture. They treat the person, not the MRI.
So what makes anyone think that the MRIs are so accurate, given that the MRVs are not seeming to be that accurate? They may be a helpful window, but maybe it's a steamy window.
Just a thought. I don't think I really expect you to be able to give an answer but really, what would make an MRI accurate if an MRV isn't?
I hope you are rested now and enjoy a beautiful day. Thank you.
But did you feel ANY better after I opened the intimal hyperplastic narrowing that you asked me to try. That was when you might have had some relief from increased blood flow. Did you?vivavie wrote:Firstly:drsclafani wrote:firstly, we must ask what was the intention behind the first intervention. Was it to eliminate some painful symptoms? to reverse some weakness or sensory mprove balance? to reverse fatigue ?vivavie wrote:If my stents are occluded what are my options, I am already on coumadin and plavix? I have a stent within stents within stents (3 layers), Is there anything more that can be done? should I even bother to get that US?
the ask whether that accomplished that. that is the first piece of the puzzle.
Secondly, if you had reversal of fortunte and symptoms returned, then was the original improvement of great value or a minor disappointing improvement.
Thirdly, what was the purpose of putting the first stent in? was it a regretful treatment plan or did it provide you with some worthwhile improvement
Fourthly, we know what the purpose of putting the last stents in. Did it provide what you were looking for.
After answering these questions, we can have a meaningful discussion of how much further to pursue this. Only you can answer these questions.
But, you are in pain, we do not know why. treatment, no treatment, i think it is important to understand what is going on because we cannot have a logical discussion with out knowing that.
drs
procedure april 2010 GOAL: relieve of pain, fatigue and hyperacousy. I have a multitude of other symptoms but they are not as debilitating, I can live with them.
In Poland the only thing done was stent at the LIJ valve - angio 3X would not stay open.
Improvements during 6 weeks: walking, bladder, bowels, saliva, swallowing, speech, headache, warm hands/feet, sweating, skin. Probably fatigue because I visited Poland for 10days - difficult to assess.
For a year now i have NO problem walking - before I could not go see a movie or ride in a car - my legs would get stiff and not move. no more limp too. But I would rather have less pain...
Second: the reversal is a Major dissapointement, 6 weeks of better life gave me hope for the futur!
I have MORE pain and fatigue, spend most of my time in bed, much less pain supine.
Third: I was nb 25 - they should not have put the stent but break down the valve. I don't think they knew better then and I certainly did not!!!
fourth: putting more stents was to prevent hyperplasia and keep the blood flowing.
I looks like there is already more hyperplasia in 2 months!!
I had a US showing little flow but no blood clot.
Question: why hyperplasia translate in soreness and swelling of the jug? It happens every time.
I do not want to have my jug shut down entirely:
1- we don't know the futur in CCSVI,
2- what happen if the rij restenosed,
3- when the vein collapsed I went thru HELL, I was declining fast. I don't think RJ and Azygos are enough for me.
You pm me about dicussing my case on TIM, please do. I may learn more and I can't open my procedure cd to see the images.
thank you for caring
nb: I wish I was better at using the quotes to answer under each of your points. did my best...
amazing....Immediately after the catheter was removed from the left saphenous vein, the patient remarked that he had improved sensation in his finger tips. In the recovery room I retested him for stereognosis. He was able to identify with his eyes closed several objects including coins, a paper clip and a penl.
Not for pain but for energy I was hopeful because just after i returned from NY we had a major fundraising event, with less manpower than we normally have. I had to do a lot of physical work for 10 days. Normally after such event I am shaking all over, can't stand myself or others and it takes me weeks to get over it. This time I was tired but not over the board. I was hopeful and thought with time and exercise I would improve but then I started to go downhill again...drsclafani wrote: But did you feel ANY better after I opened the intimal hyperplastic narrowing that you asked me to try. That was when you might have had some relief from increased blood flow. Did you?
Why do you react so badly to stents. Some people just do. I wish i could predict better. Some people just form exhuberant scar tissue.
i guess the only other consideration if the intimal hyperplasia does not subside might be to put in a covered stent to prevent the intimal hyperplasia from growing through the stent wires. But if opening the stents didnt help by providing short term increased blood flow, i am not sure what we would be accomplishing.
Dr Makris is a well trained, former academic interventional radiologist, who has chosen to go into private practice at american access. His practice is practically 100% venous disease. Although he is relatively new to CCSVI treatment, he has done thousands of venous angioplasties. He has a very busy practice and cannot devote more time to ccsvi at the moment until he recruits and hires a partner.cowboystew wrote:Hi Dr. S,
Do you share information with the IR at American Access Care in Chicago? I'm going there for treatment May 10 - 11. This will be round 2 for me, and I'm hoping for results that last longer than my first time (17 days). Can you tell me anything about this doctor? Does he keep up with new discoveries? I was the first CCSVI patient of my South Bend doctor. I'm getting nervous, and I need to feel like I'm in good, experienced hands. ~Nancy
Outside of your practice, is it common or uncommon for ccsvi IRs to image the azygos in different angles like this?drsclafani wrote:
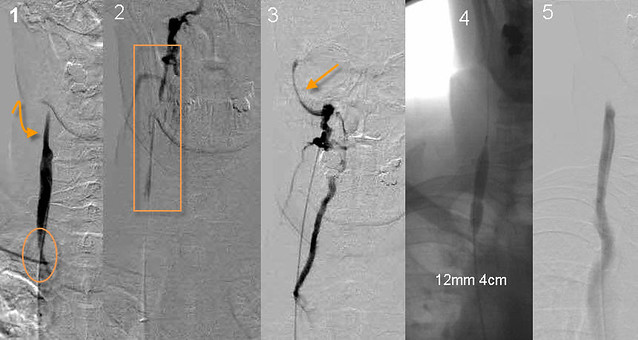
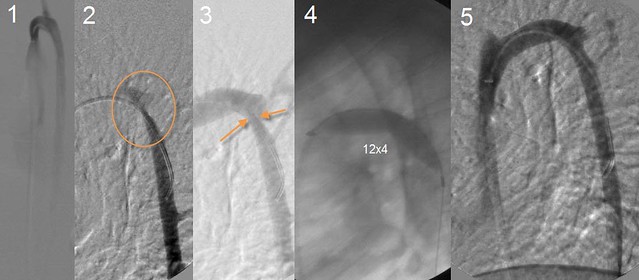
This azygous venography is really illustrative of several points. Firstly, the frontal view (#1) looks normal. No stenosis. On the 70 degree view Fig #2,3), the posterior part of the azygous arch is beautifully seen and there is a significant stenosis.
My patern has been to develop hyperplasia within 6-8 weeks each time. You choose to installed 2 layers of mesh stents inside my actual stents over ONE covered stent. Why? there must be some disadvantages to the covered stents.drsclafani wrote: ... Some people just form exhuberant scar tissue.
i guess the only other consideration if the intimal hyperplasia does not subside might be to put in a covered stent to prevent the intimal hyperplasia from growing through the stent wires...