Page 328 of 557
Posted: Tue Apr 19, 2011 11:24 am
by davmets2
drsclafani wrote:
You are indeed fortunate that your thrombosis was able to reverse itself while on coumadin. Often, occlusion of the jugular vein is a permanent thing. You might not have had such an outcome if this vein had been the second vein treated rather than the first one.
I think that the ultrasound examination is the best screening test. Cheap, accurate and to the point.
Now you want to know how much flow there in within the vein? I would personally want to perform a venogramto assure that the vein interpreted as the IJ, actually was the IJV. Sometimes collateral vessels get quite large and may look very much like the internal jugular.
If the vein is narrowed significantly, I would try angioplasty with the expectation that a stent might be needed.
What possibly could be causing all the thromboses that we hear about. I wonder what percentage of patient treated develop IJ thrombosis.
I know that the cases of thrombosis that i have been involved with come in two forms.1. Overdilation of veins and very high pressures in relatively normal veins. Choosing vein diameter is much more precise using IVUS. I havent had a thrombosis since changing my procedure. The other association is with thrombosis resulting from treatment of hypoplastic veins. That is the reason that I have backed off aggressive treatment of hypoplasias..
Thanks for answering my question.
I guess what you're suggesting to me is that I should have a venogram done if I'm not satisfied with the US interpretation and the results I recieved with the procedures I had done. I have a feeling that an 18mm balloon was probably bigger than what should have been used due to not having the accuracy of IVUS, thus possibly causing the thombosis that occurred. When I looked at the before and after size of the LIJ, it looked quite larger after the first procedure. I'd post them with snagit, but don't know how to.
Posted: Wed Apr 20, 2011 5:56 am
by drsclafani
Cece wrote:drsclafani wrote: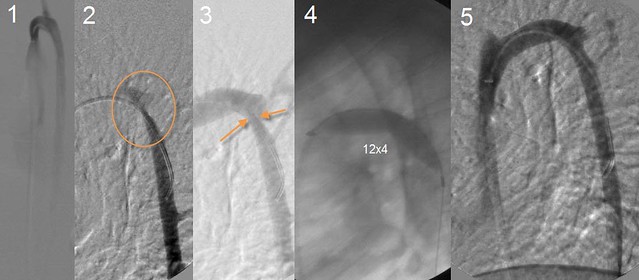
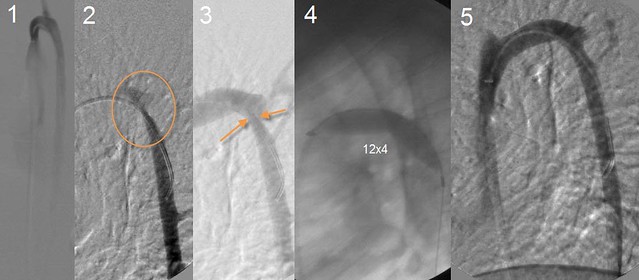
This azygous venography is really illustrative of several points. Firstly, the frontal view (#1) looks normal. No stenosis. On the 70 degree view Fig #2,3), the posterior part of the azygous arch is beautifully seen and there is a significant stenosis.
Outside of your practice, is it common or uncommon for ccsvi IRs to image the azygos in different angles like this?
i havent noticed anyone speak about it.
That azygous is a real challenge. We have talked about it before.
i used to do 0 degrees, 20 degrees, 70 degrees, 90 degrees until i had a decent understanding of which views offered the most information.
My standard routine currently is to perform an inhalation breathhold, AP view to look at the ascending portion of the azygous vein. I do an upper and a lower view trying to see the entire azygous, hemiazygous and connections to the renal vein. Then I do a 70 degree oblique. With a 70 degree oblique, i do not h ave to raise the arms above the head. It is good in about 90% of cases in seeing the entire arch of the azygous and giving a second view of the ascending azygous. If either the anterior or posterior arch is not well visualized or obscured by superimposition, I will do a 90 degree view. that usually suffices. Then I do IVUS because I do not trust the venogram 100% in most cases.
Posted: Wed Apr 20, 2011 5:59 am
by Rokkit
So far, what percentage of patients are you finding with azygous stenosis?
Posted: Wed Apr 20, 2011 6:00 am
by drsclafani
vivavie wrote:drsclafani wrote:
... Some people just form exhuberant scar tissue.
i guess the only other consideration if the intimal hyperplasia does not subside might be to put in a covered stent to prevent the intimal hyperplasia from growing through the stent wires...
My patern has been to develop hyperplasia within 6-8 weeks each time. You choose to installed 2 layers of mesh stents inside my actual stents over ONE covered stent. Why? there must be some disadvantages to the covered stents.
Is there enough room to insert a covered stent? that would make it 4 layers?
I ask my question here for the benefit of other patients with similar problem.
It has been our experience that adding layers of metal has worked to get control. but that experience was with hemodialysis veins. A series of one does not prove anything, but i would be skeptical about trying this again.
Covered stents are more expensive and less anchored.
Posted: Wed Apr 20, 2011 6:08 am
by drsclafani
davmets2 wrote:drsclafani wrote:
You are indeed fortunate that your thrombosis was able to reverse itself while on coumadin. Often, occlusion of the jugular vein is a permanent thing. You might not have had such an outcome if this vein had been the second vein treated rather than the first one.
I think that the ultrasound examination is the best screening test. Cheap, accurate and to the point.
Now you want to know how much flow there in within the vein? I would personally want to perform a venogramto assure that the vein interpreted as the IJ, actually was the IJV. Sometimes collateral vessels get quite large and may look very much like the internal jugular.
If the vein is narrowed significantly, I would try angioplasty with the expectation that a stent might be needed.
What possibly could be causing all the thromboses that we hear about. I wonder what percentage of patient treated develop IJ thrombosis.
I know that the cases of thrombosis that i have been involved with come in two forms.1. Overdilation of veins and very high pressures in relatively normal veins. Choosing vein diameter is much more precise using IVUS. I havent had a thrombosis since changing my procedure. The other association is with thrombosis resulting from treatment of hypoplastic veins. That is the reason that I have backed off aggressive treatment of hypoplasias..
Thanks for answering my question.
I guess what you're suggesting to me is that I should have a venogram done if I'm not satisfied with the US interpretation and the results I recieved with the procedures I had done. I have a feeling that an 18mm balloon was probably bigger than what should have been used due to not having the accuracy of IVUS, thus possibly causing the thombosis that occurred. When I looked at the before and after size of the LIJ, it looked quite larger after the first procedure. I'd post them with snagit, but don't know how to.
its not just whether you like the interpretation of the US. The US should tell us whether there is flow. if there is flow, there is a chance to salvage the vessel. If there is a chance, you have to perform a venogram to be sure what you are dealing with and you h ave to get a guidewire across the area that might be narrowed. in other words, you have to connect the dots. once a guidewire is across, you might be able to get this vein open, although the restenosis rate or thrombosis rate might be higher than simple angioplasty of a clean vessel., but probably better than re-angioplasty of an area of thrombosisl.
Posted: Wed Apr 20, 2011 6:12 am
by drsclafani
Rokkit wrote:So far, what percentage of patients are you finding with azygous stenosis?
25% estimate.
Incidence seems to be going up, or rather diagnosis seems to be going up, probably because of IVUS and more confidence that some observations initially thought to be normal are not normal.
i am also seeing things on IVUS that i am not sure of. High intensity signals in random areas. Are they webs? Do not yet know what to do with those.
Still in age of discovery, i guess. But the discoveries are more nuanced now.
Posted: Wed Apr 20, 2011 10:58 am
by bluesky63
Forgive me if you've already talked about this, but I am curious if you have found a pattern in your own procedures that correlates with disability. You mentioned about 25 percent azygous abnormaility. Do you find that azygous dysfunction means more severe disability? Or that particular patterns of abnormalities correlate with patterns of disease/disability? Or even recovery or procedure effectiveness?
I'm sorry if I'm throwing too much into one post here. It's so exciting to think anything might make sense in this crazy disease. Thank you for any insight.

Posted: Wed Apr 20, 2011 6:49 pm
by drsclafani
bluesky63 wrote:Forgive me if you've already talked about this, but I am curious if you have found a pattern in your own procedures that correlates with disability. You mentioned about 25 percent azygous abnormaility. Do you find that azygous dysfunction means more severe disability? Or that particular patterns of abnormalities correlate with patterns of disease/disability? Or even recovery or procedure effectiveness?
I'm sorry if I'm throwing too much into one post here. It's so exciting to think anything might make sense in this crazy disease. Thank you for any insight.

sorry, i havent recognized any pattern at all.
Posted: Thu Apr 21, 2011 6:41 pm
by Cece
drsclafani wrote:i havent noticed anyone speak about it.
That azygous is a real challenge. We have talked about it before.
i used to do 0 degrees, 20 degrees, 70 degrees, 90 degrees until i had a decent understanding of which views offered the most information.
My standard routine currently is to perform an inhalation breathhold, AP view to look at the ascending portion of the azygous vein. I do an upper and a lower view trying to see the entire azygous, hemiazygous and connections to the renal vein. Then I do a 70 degree oblique. With a 70 degree oblique, i do not h ave to raise the arms above the head. It is good in about 90% of cases in seeing the entire arch of the azygous and giving a second view of the ascending azygous. If either the anterior or posterior arch is not well visualized or obscured by superimposition, I will do a 90 degree view. that usually suffices. Then I do IVUS because I do not trust the venogram 100% in most cases.
I love the images, it is something to see how the azygous looks ok in the first view and then the stenosis is seen in the "side view."
We've heard recently that another CCSVI doctor has been finding and treating renal vein obstructions too. What do you think of this? Have you seen any renal vein obstructions and have you looked?
Posted: Fri Apr 22, 2011 4:30 am
by Liberation
,,,,,,,,,,,,,,,,,,,,,,
Posted: Fri Apr 22, 2011 6:04 am
by Cece
Liberation wrote:drsclafani wrote:Cece wrote:tzootsi, that caught my attention! If you follow tzootsi's link, quick summary is that Vitamin D3 is bad after an endovascular procedure (if you are a rat) because it increases the amount of intimal hyperplasia. Eeep.
Wonderful news.
With hyperplasia, isn't leaving it alone currently the best option? These veins may only be taking a very small amount of flow, but we need whatever flow we have, and the track record for success is at null as far as I know.
anticoagulation and antiplatelet therapy could help.
I just reread that, I meant 'hypoplasia' when I said 'hyperplasia.' Changes the answer completely.
First, only a 1cm section went back to the position where it was before the operation, then a month later the IR told me that the full length restenosed. I do not know how I can find out it is a recoil or hyperplasia.
Do you have any images to post?
It's odd to hear it described as a '1 cm section' and then the full length. It does not sound like the IR was considering this a disease of the valves, since he is talking about the full vein. Do you know if he ballooned the valves? Since small balloons were used, recoil would seem like a strong possibility. Most hyperplasia cases that I can remember have involved stents.
Posted: Fri Apr 22, 2011 1:07 pm
by Liberation
[...............
Posted: Fri Apr 22, 2011 6:33 pm
by Brainteaser
Liberation wrote:Now, I hold out more hope for dr Sclafani's approach with ivus. I still do not understand why others do not use it, it sounds a brilliant idea.
Is cost the issue? Someone raised ivus with Prof Thomson in Melbourne (public hospital system) and I think this was the reply.
Posted: Fri Apr 22, 2011 6:54 pm
by Cece
I have heard only of Dr. Sclafani, Dr. Dake, Dr. Haskal, Dr. Cumming and Dr. Arata ever using IVUS for CCSVI. (This is by memory: Dr. Sclafani, obviously; Dr. Dake, using IVUS to find a stenosis in CUREious that regular venogram had missed; Dr. Haskal, can't quite remember; Dr. Cumming, from statements here at TIMS; Dr. Arata, double-checked and found this post about him using IVUS at the hospital for May Thurner cases and wanting it at the clinic but too expensive:
www.thisisms.com/ftopicp-132203.html#132203).
It is brilliant. Dr. Sclafani presented on it at ISNVD. I am hoping for a publication sooner or sooner. Or later, if need be.

Expensive unit, expensive single-use catheters, learning curve (not as useful to doctors who are not as good at using it) and higher amortization costs due to less frequent usage, on one hand. Added info and reduced risk to the patient, on the other hand.
Posted: Fri Apr 22, 2011 7:18 pm
by bestadmom
To add to CeCe's spot-on explanation of why IVUS isn't widely used, currently it is not reimburseable thru insurance. When Dr. S uses it, AAC pays for it, not the patient. It's at least a $600 catheter expense. Then there's the time involved to examine the veins two ways, and the equipment to view the images.