Page 346 of 557
Posted: Mon May 30, 2011 7:17 am
by pklittle
First high pressure angioplasty was performed at the confluens with the subclavian vein. Then the sigmoid sinus was flushed with heparinized saline Then suction was applied to the jugular bulb. .Finally, a thrombus was aspirated from the internal jugular vein. This thrombus appeared dark and dense and i believed it was old thrombus. .After these three maneuvers, there was brisk flow in the internal jugular vein.
Did the saline flush help in extracting the thrombus? I am so happy to read you were able to get the thrombus out and restore flow.
I ask all my patients to come for an "E-visit" once per month so i can see how they are doing. Not all keep their visits but quite a few do. The rest? I am coming after you.
Am I ready? I don’t know. Maybe? We consulted in February. I’m certainly not getting any better... but my fear is of getting more occlusions/damage than I already have from a prior treatment.

Posted: Mon May 30, 2011 8:16 am
by Cece
drsclafani wrote:pklittle wrote:Another question: Have you just recently learned that changing positions/turning the head can impact flow?
no. But i havent found it very commonly. This was the nicest example. When i find narrowings in the J2 segment, i am skeptical. My main goal is determining whether this is a fixed narrowing or whether it is dynamic. Most are dynamic.
Dr. Haskal had some dramatic images of this at ISET.
(see p.16, p.30) (these presentations are accessible through google search but weren't intentionally published by the doctors.)
http://tinyurl.com/3ergfjg
Posted: Mon May 30, 2011 8:54 am
by Donnchadh
What an amazing journey MS patients and their treating doctors have undertaken together! I viewed your latest case report and could actually understand what you were doing, where, and why. The Internet has enabled a whole new type of patient to emerge: much more informed and active in determining what treatment options are available to them.
And dear doctor you are setting a very high standard for others to follow!
Not just for your fine work on the operating table, but also for educating the public and patients affected by this damn disease.
Thank you so very much.
Donnchadh
Re: DrSclafani answers some questions
Posted: Mon May 30, 2011 9:17 am
by Cece
PCakes wrote:For those living alone yet longing to benefit from your gift, might there be a volunteer like group in Brooklyn that could be contacted to supply patient companion/assist?
I'd worry that this would encourage people to come alone and that it wouldn't be enough unless it was around-the clock assistance. I'm reminded of LadyGazelle's experience, discussed here in this thread many months back and in her blog, where her femoral artery had been mistakenly punctured and plugged, and back at the hotel room the plug came loose, and a lot of bleeding ensued, and she too was travelling alone.
Re: DrSclafani answers some questions
Posted: Mon May 30, 2011 10:04 am
by PCakes
Cece wrote:PCakes wrote:For those living alone yet longing to benefit from your gift, might there be a volunteer like group in Brooklyn that could be contacted to supply patient companion/assist?
I'd worry that this would encourage people to come alone and that it wouldn't be enough unless it was around-the clock assistance. I'm reminded of LadyGazelle's experience, discussed here in this thread many months back and in her blog, where her femoral artery had been mistakenly punctured and plugged, and back at the hotel room the plug came loose, and a lot of bleeding ensued, and she too was travelling alone.
..but Cece, what of those who don't have someone? Most will have to travel even while staying as close to home as possible. That's why I ask if there might be a volunteer group that might offer a companion service?
Anything is possible..

pc
Re: DrSclafani answers some questions
Posted: Mon May 30, 2011 12:30 pm
by drsclafani
PCakes wrote:Cece wrote:PCakes wrote:For those living alone yet longing to benefit from your gift, might there be a volunteer like group in Brooklyn that could be contacted to supply patient companion/assist?
I'd worry that this would encourage people to come alone and that it wouldn't be enough unless it was around-the clock assistance. I'm reminded of LadyGazelle's experience, discussed here in this thread many months back and in her blog, where her femoral artery had been mistakenly punctured and plugged, and back at the hotel room the plug came loose, and a lot of bleeding ensued, and she too was travelling alone.
..but Cece, what of those who don't have someone? Most will have to travel even while staying as close to home as possible. That's why I ask if there might be a volunteer group that might offer a companion service?
Anything is possible..

pc
This is a generous and thoughtful idea. While an overnight alone is not encouraged, risks are pretty low. Call me just cautious.
however the procedure is stressful and i cannot imagine most patients spending the night alone. why chance it
Posted: Mon May 30, 2011 12:34 pm
by drsclafani
drsclafani wrote:
i still have this great case to share and still waiting for notjohnson to resurface
DrS
Case shared.
notjohnson resurfaced long enough to tell me he didnt have good internet availablity, is fine and will come out of hibernation shortly
Posted: Mon May 30, 2011 12:49 pm
by Cece
But did you get outside and enjoy a beautiful day?

Who knows what the next week holds!
NotJohnson has posted here and all is well:
www.thisisms.com/ftopicp-166688.html#166688
Posted: Mon May 30, 2011 4:32 pm
by Cece
drsclafani wrote:
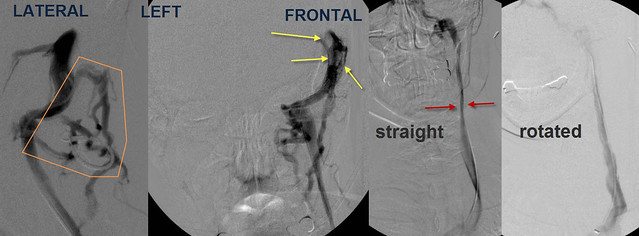
Figure A shows narrowing of the J2 segment. When i asked the patient to turn her head to the left and repeated venography (Figure B), the vein looks normal. the collaterals are not visualized.
Really clear images. I would not have expected this to be from the same patient.
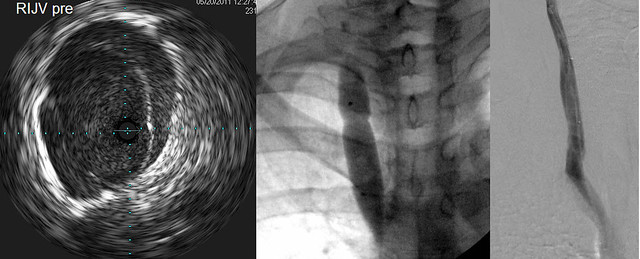
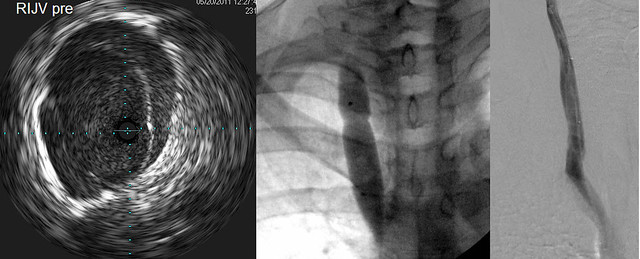
IVUS (left) showed a thickened valve which did not completely open at any time during interrogation.
Angioplasty (center) showed a modest narrowing in the balloon at nominal pressure.
Post procedural angioplasty (right) showed improved flow
Am I interpreting this right that ballooning of the valve was enough to improve the flow higher up, where it had been compressed by a muscle?
Posted: Mon May 30, 2011 4:40 pm
by Cece
drsclafani wrote: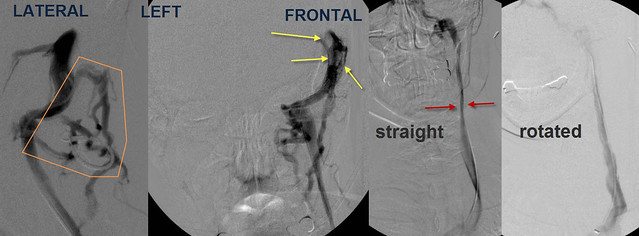
Selective catheterization and venography of the left sigmoid sinus showed that unlike the right side extensive collateral veins were noted in the back of the neck (orange) Also noted were filling defects, consistent with thrombus, in the sinuses. Frontal venogram of the L IJV showed narrowing in J2 (red arrows) similar to the right side. Again, upon rotation of the neck, flow was improved and diameter was normal.
Will there be any treatment for the patient's sinus thrombosis?
Did the patient have any symptoms of sinus thrombosis or a guess as to when it occurred in the patient history?
Was there any external/physical appearance to the neck to suggest the problematic muscles? Was CTOS discussed? Could neck stretches help these muscles loosen up?
Posted: Mon May 30, 2011 4:53 pm
by Cece
drsclafani wrote:First high pressure angioplasty was performed at the confluens with the subclavian vein. Then the sigmoid sinus was flushed with heparinized saline Then suction was applied to the jugular bulb. Finally, a thrombus was aspirated from the internal jugular vein. This thrombus appeard dark and dense and i believed it was old thrombus. After these three maneuvers, there was brisk flow in the internal jugular vein.
Amazing.... Why was this thrombus removable when others aren't? Just luck or bad luck, in the contrary situation?
Would every IR approach this by flushing with heparinized saline and applying suction? Or were there other choices you could have made?
Did the pre-existing thrombus blockage in the sinus cause slow flow and made it more likely for the thrombus in the jugular to form?
If the patient is thrombus-prone, will she be getting a one-month follow-up ultrasound?
Posted: Mon May 30, 2011 5:02 pm
by Cece
drsclafani wrote:So first i looked at the left renal vein:

The green arrow points to the catheter in the renal vein. There is no contrast in the renal vein. rather the renal vein drains through the hemiazygous vein and outlines all the lumbar veins and the vertebral plexus.
This is a tremendous amount of blood to add to the azygous vein and vertebral plexus. The left renal vein drains about 500 ml of blood/minute. The entire brain drains approximately 750 ml of blood/minute. Thus this venous obstruction almost doubles the blood in the cerebrospinal blood pool, not good when the aygous and its collaterals, and the the internal jugular veins have stenoses!
500 ml/minute!
I am a bit aghast, I did not know the renal vein drained that much. Previously you had said you'd found one case of renal stenosis, now it presumably is just two cases out of 150. But when found, it is significant.
I can check google scholar for this myself but it's a question raised: what is typically done for renal vein stenosis? Is this an uncommonly treated area or is there a body of research on it?
I know there is controversy in whether to stent or not stent the iliac vein. I have heard very little about the renal vein.
Posted: Mon May 30, 2011 5:15 pm
by Cece
drsclafani wrote:So that is how i spend my time.
I cannot imagine a more worthwhile or enduring use of your time and skills.
Except not so much the cab ride thing...but that was very generous, not just to go the extra mile, but to literally go a few extra miles.

Key points
1. IVUS finds things that are unrecognizable by venography
Remember when the venogram of my azygous looked really good and you decided not to use IVUS on it? I have wondered (and sometimes worried), would you still make that same decision today?
2. the dural sinuses may cause compromised outflow. Whether MRV or venography are superior is unclear to me. At any rate one or the other probably should be part of the investigation of ccsvi
3. This is not likely restenosis but underdilation and elastic recoil because of the time frame
4. The renal vein is an important vessel to study, especially when the aygous is compromised. The renal vein and the ascending lumbar vein form an important collateral drainage pathway when the azygous is stenosed or they can add stress on the cerebrospinal venous circulation when their normal outflow is compromised.
Any questions?
Posted: Mon May 30, 2011 6:41 pm
by drsclafani
Cece wrote:drsclafani wrote:So first i looked at the left renal vein:

The green arrow points to the catheter in the renal vein. There is no contrast in the renal vein. rather the renal vein drains through the hemiazygous vein and outlines all the lumbar veins and the vertebral plexus.
This is a tremendous amount of blood to add to the azygous vein and vertebral plexus. The left renal vein drains about 500 ml of blood/minute. The entire brain drains approximately 750 ml of blood/minute. Thus this venous obstruction almost doubles the blood in the cerebrospinal blood pool, not good when the aygous and its collaterals, and the the internal jugular veins have stenoses!
500 ml/minute!
I am a bit aghast, I did not know the renal vein drained that much. Previously you had said you'd found one case of renal stenosis, now it presumably is just two cases out of 150. But when found, it is significant.
I can check google scholar for this myself but it's a question raised: what is typically done for renal vein stenosis? Is this an uncommonly treated area or is there a body of research on it?
I know there is controversy in whether to stent or not stent the iliac vein. I have heard very little about the renal vein.
Thanks for asking
yes i have now two cases. both have azygous disease.
The first patient had very very short lived clinical improvements before things got worse.
I did not treat the renal vein because i thought that i needed to do further workup before i addressed it.
the usual workup includes a urinalysis for red blood cells, protein. checks of blood pressure which may be elevated. queries regarding back pain, and pelvic pain.
Computed tomography is recommended for futher evaluation of the number of veins, and their locations.
the usual cauases of this type of obstruction is compression due to adjacent tumors and lymph nodes, compression between the aorta and the superior mesenteric artery (NUTCRACKER SYNDROME), or aberrant location of the renal vein behind the aorta (RETROAORTIC RENAL VEIN) or the vein splits into two with one going behind and one going in front of the aorta (CIRCUMAORTIC RENAL COLLAR).
Treatments include surgical disentanglement by moving these major veins and resuturing in a way that takes the pressure off, or nephrectomy, or stenting. Stenting has come into favor because it is so much less invasive.
another cause is thrombosis of the renal vein. This is much less likely to occur
i think that these are truncal malformations in many circumstances wheree the veins of the fetus malform during transition between the fetal veins and the adult veins.
Posted: Mon May 30, 2011 6:45 pm
by drsclafani
Cece wrote:drsclafani wrote:
Figure A shows narrowing of the J2 segment. When i asked the patient to turn her head to the left and repeated venography (Figure B), the vein looks normal. the collaterals are not visualized.
Really clear images. I would not have expected this to be from the same patient.
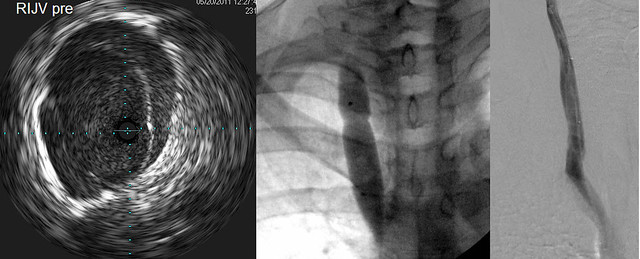
IVUS (left) showed a thickened valve which did not completely open at any time during interrogation.
Angioplasty (center) showed a modest narrowing in the balloon at nominal pressure.
Post procedural angioplasty (right) showed improved flow
Am I interpreting this right that ballooning of the valve was enough to improve the flow higher up, where it had been compressed by a muscle?
I think that muscle comrepssion is common. Some get it when they turn their heads. others get it when their head is straight. I think these are likely physiological narrowings. i would never treat one on the first treatment. If things didnt get better, then i would consider treatment. but that treatment might entail a stent (ughh)