Cece wrote:drsclafani wrote:i have thought about traversing the dural sinuses to go from one side to another. At the current time, I consider this to be beyond my technical expertise. I would seek the assistance of a interventional neuroradiologist who has experience with this treatment. I would imagine that this would be unlikely to be successful.
That seems wise.
Although I wish there was a interventional neuroradiologist convinced of the merits of ccsvi and knowledgeable of our particular issues. All in good tme, I suppose, and as the research comes in.
Any interesting cases lately?
Well, now that the symposium is completed, i have had some time to think about interesting and informative cases.
Monday was a rough day starting at 730am and ending at 1030pm. each case was noteworthy. and there are some interesting associations.
let's review the first patient. I am putting myself out there for this one, as you will see that my logic dictated that i treat this patient in stages.
history: A 44 year old British woman living in Greece came to me one year after initial treatment of CCSVI in Greece. Officially diagnosed with MS in 2005, she sustained optic neuritis in 1983. Her primary complaints include numbness in her lower torso and lower extremities, painful spasticity of her legs, weakness in both lower extremities and left arm and urinary urgency. Her EDSSS was 7.0.
She had convinced an interventional radiologist in Greece to investigate her veins. He performed venography, stated that there were mild narrowings and decided that there was no stenosis worthy of angioplasty.
One year later this patient consulted me. As we moved toward a visit from Greece to New York with an appointment for venography and possible venoplasty or valvuloplasty, we came across an impediment to performing the procedure. It is my practice to anticoagulate patients for a few weeks after angioplasty with an anti thrombin a medication such as fondaparinux or dabigatran . This patient was concerned because she suffers from menorrhagia, a condition of excessive hemorrhage during menstruation. It is commonly seen in perimenopausal women with uterine fibroid tumors, which can also can cause anemia, require transfusions, and press on the bladder to cause urinary frequency and urgency and constipation. Patients sometimes also experience pain during sexual intercourse.
The solution we arrived at was to perform UFE, transcatheter particulate embolization of the uterine arteries that supply blood to the fibroids. By blocking these blood vessels, the fibroids are deprived of oxygen and nutrients and thus die. Bleeding is controlled and patients have improved quality of life, eliminating excessive bleeding in a one hour minimally invasive alternative to hysterectomy and allowing anticoagulation with less risk.
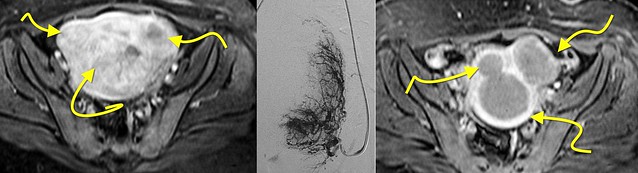
I do not have good images from this case but here is an example of a UFE.
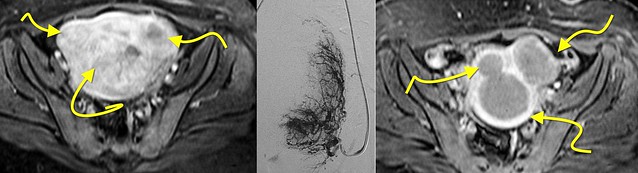
on the left is an MRI of a uterus filled with large fibroids (yellow arrows). The middle image shows a arteriogram with the catheter in the uterine artery. The darkish areas represent blood flow to very vascular fibroids. On the right is a followup MRI of the uterus. Note how the fibroids now have a dark center devoid of blood flow.
So we treated the fibroids in my patient on Monday and brought the patient back the next Monday for CCSVI procedure. The usual venogram includes catheterization of the right and left transverse sinuses, the right and left internal jugular veins, the azygous vein, the left renal vein, the left iliac vein and the left ascending lumbar vein.
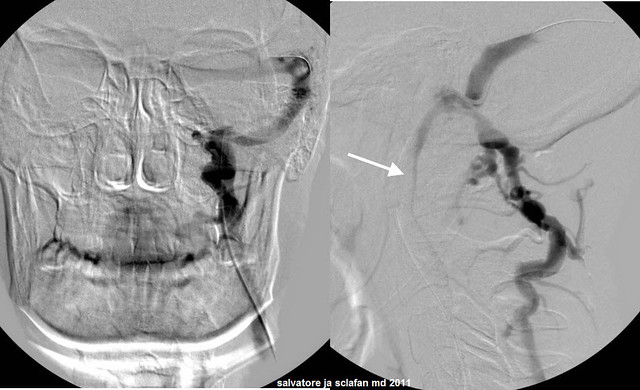
LEFT DURAL SINUS VENOGRAM
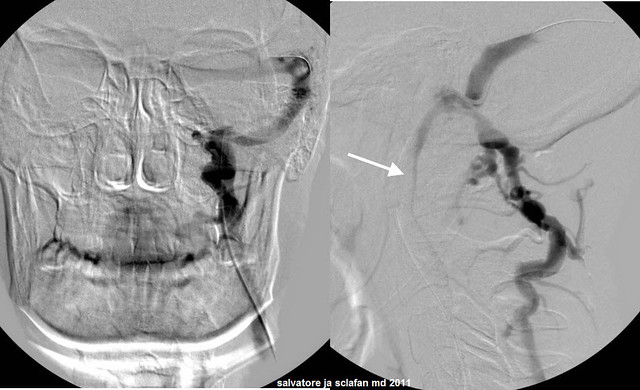
The venogram showed an intact transverse and sigmoid sinuses, free of thrombus and webs. However the flow into the jugular vein is limited and blood flows preferentially into the vertebral vein. This is opposite of normal blood flow which should be through the IJV when lying down. Why should this occur? Such reversal of flow is usually an outflow problem. The IJV is barely opacified. Note the jugular narrowing (white arrow) at the second cervical vertebra. This is a challenging area of narrowing.
I was concerned. This is not a typical location for malformation of the veins and is more likely a problem of venous compression. Angioplasty of such lesions usually reveals no "waist" on the balloon and IVUS usually shows that this area is distensible and expandable. Generally I remain unclear whether this narrowing is treatable or should be treated. The consideration for treatment will be stenting because the problem is compression of the vein against the spine. Stenting in this area is associated with some serious complications including injury of the spinal accessory nerve. Before making such a decision it is important to evaluate the entire jugular vein.
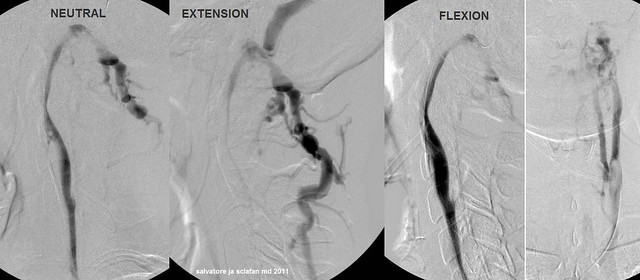
UPPER INTERNAL JUGULAR VEIN
So let's look at what the IJV looks like as we change the muscle compressions against the spine. The vein is imaged in a neutral, a flexion and an extension position.
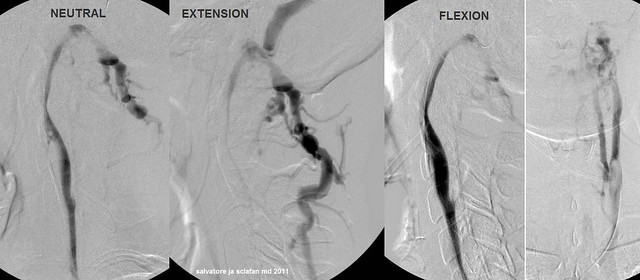
As you can see, the narrowing is related to position of the neck. When in the neutral position it is compressed. When the neck is placed in full extension, the narrowing is greater and the collaterals are larger. it is interesting to see that flexion of the neck leads to reduction in the compression, improvement in flow and reduction of vertebral collateralization.
What will ultimately be recommended for such lesions is unclear at this time. On the first treatment, I decided NOT to treat by angioplasty or stenting. We will see how this patient does with standard treatments and then decide what to do about this in the future as we see how she responds.
So discussion number one. Should I have stented this vein?
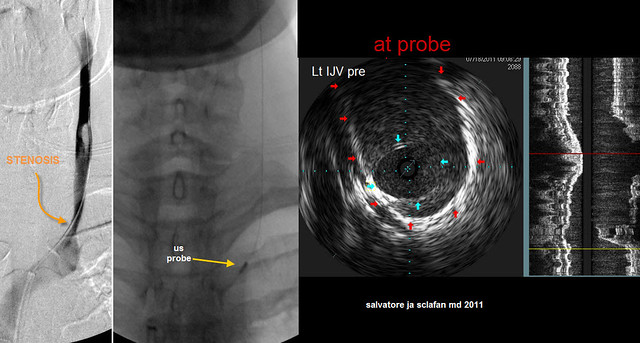
LEFT JUGULAR VEIN
The rest of the IJV was also a challenge. Flow was slow and collaterals were visible. There was a slight narrowing of the lower end of the vein over a couple of centimeters
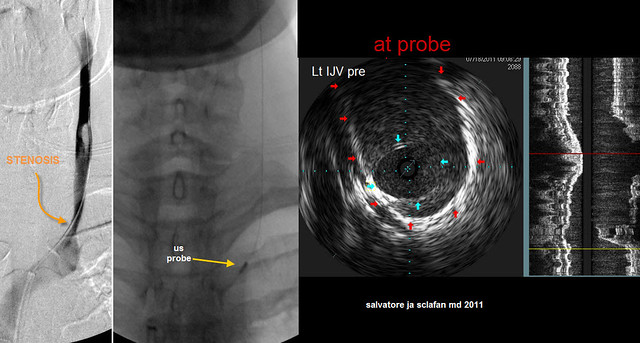
On the left image, there is a mild looking stenosis (curved orange arrow) that looks rather subtle. to the right of this a yellow arrow points to the ultrasound probe. The right of that is an IVUS image at the probe. The blue arrows point to the edges of a stenotic valve. The lumen of the valvular area is quite small compared to the full diameter of the vein (red arrows outline it). I estimate the narrowing to be at least 75%. It is clear that the IVUS does a better job of evaluating the stenosis and illustrating the pathology.
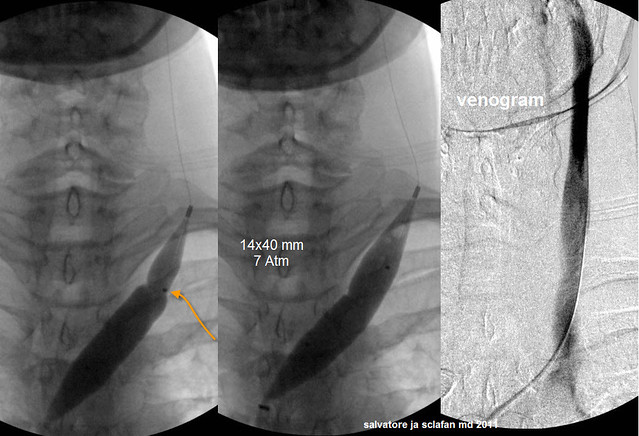
TREATMENT OF LOWER LEFT INTERNAL JUGULAR STENOSIS
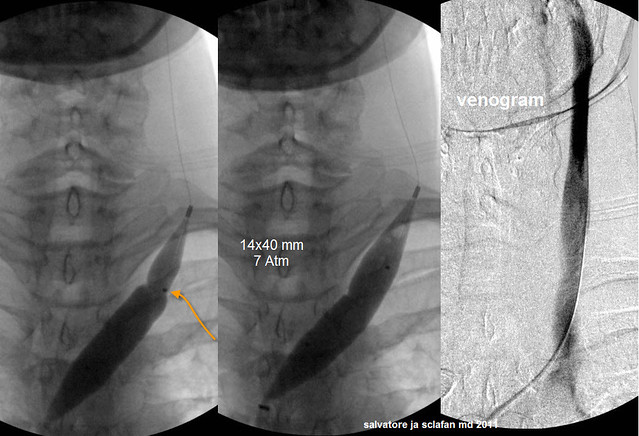
This valvular stenosis was treated with a 14 millimeter balloon which, when inflated, has a surface area about 50% greater than the full vein wall. Since the vein is larger below the stenotic valve, the balloon is positioned eccentrically with the majority of the balloon below the valve. This prevents stretching the normal vein. At 7 atmospheres the waist on the balloon was eradicated and there was no elastic recoil noted.
The image on the right shows improved diameter and improved faster flow.
RIGHT INTERNAL JUGULAR VEIN
The procedure then studied the right internal jugular vein. This was not shown here. FLow was excellent and no stenosis or valvular problems, webs or septum was seen.
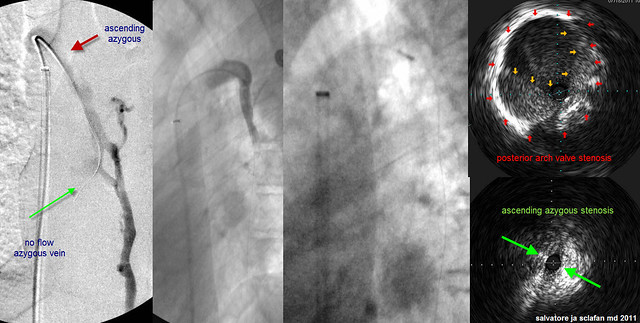
AZYGOUS VEIN
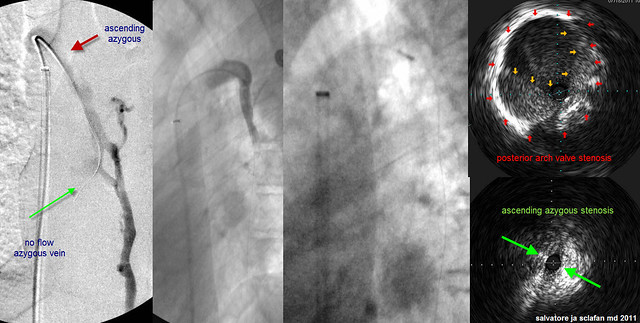
The left image shows the azygous vein in the frontal view. Notice how one cannot really evaluate the arch of the azygous which is m uch better seen in a steep oblique of "off" lateral. There is reflux in the hemiazygous vein but there is no flow down the azygous vein (green arrow). Other collateral veins are also seen. The upper portion of the ascending azygous vein (red arrow) is poorly seen and likely there is obstruction there.
The image to the right of this first image is a more detailed view of the area in question. There does appear to be stenosis of the azygous in its ascending portions. The third image shows the ultrasound probe in the area of the posterior azygous arch. The final image shows two abnormalities. In the upper image there is a posterior valve stenosis. The yellow arrow points to the edges of a fixed valve. The red arrows point to the edges of the vein itself. I estimage this stenosis to be about 50%. The lower image shows the stenosis of the lower azygous (ascending portion)The lumen was completely closed down and this did not expand with respiration.
AZYGOUS TREATMENT

Therefore a short balloon was placed in the arch of the azygous. One can see the waist in the balloon on nominal pressures. At ten atmospheres of pressure this stenosis was opened. Followup image shows the arch better but there is still no flow in the ascending azygous. A balloon was inflated along the majority of the ascending azygous. Angioplasty had NO effect on this stenosis and there was still no flow. So a stent was placed in order to get some flow. I would prefer not to use stents but failure of repeated angioplasty to open up a vein is one of my indication to stent. Followup venography (far right) shows improved flow.
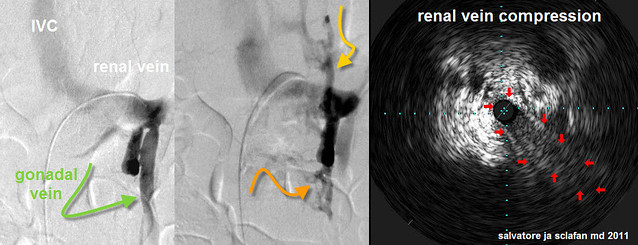
LEFT RENAL VEIN
I now image the left renal vein in all cases because of the great blood flow within it. When there are outflow problems with this vein, a major collateral circuit is to the ascending lumbar vein (increasing flow through vertebral plexus) and to the hemiazygous vein (contributing greatly to the azygous system. There are two anomalies that typically obstruct left renal vein outflow: the nutcracker compression of the vein between the superior mesenteric artery and the abdominal aorta and retroaortic renal vein that can get compressed against the spine and back.
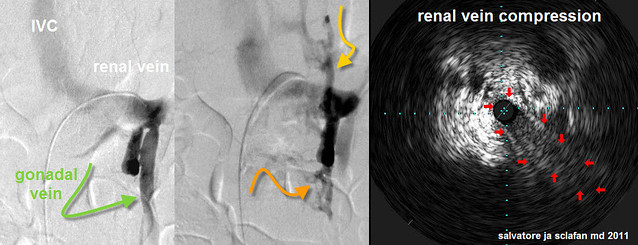
The image on the left shows the catheter going from the inferior vena cava into the left renal vein. There is an area of minimal xray dye in the middle of the renal vein. The gree curved arrow points to the ovarian vein. It is not common to see so much contrast media entering it. The next image shows that in addition to the gonadal vein, there is reflux into the ascending lumbar vein (orange arrow) and the hemiazygous vein (yellow arrow). THIS IS NOT NORMAL. The image on the right is an IVUS image of the renal vein. The renal vein is compressed (red arrows). I bet Nutcracker syndrome. Does treatment of this syndrome improve symptoms of ccsvi? I will review soon another patient who had already been treated for CCSVI (BUT NOT NUTCRACKER) who has already shown improvements of the prior CCSVI treatment.
LEFT ILIAC VEIN AND INFERIOR VENA CAVA and LEFT ASCENDING LUMBAR VEIN
We image the left iliac vein and inferior vena cava for two purposes: firstly we want to exclude compression syndromes of the left common iliac vein. Known as the May Thurner syndrome, this stenosis is caused by compression of the left iliac vein against the spine by the iliac artery that crosses it. It cannot happen on the right side. Venous outflow of the left leg is through collaterals including the internal ilac vein and the ascending lumbar vein.
May Thurner syndrome is a variant anatomy occuring in 2-5% of the general population. Symptoms include deep vein thrombosis of left leg. However not all patients with compression have symptoms. MTS is not more frequent in PwMS but is syndrome is important toCCSVI because increased flow through the ascending lumbar vein adds circulation to the compromised cerebrospinal venous circulation.

This is a perfect storm, not only left jugular and azygous stenoses but compressions of BOTH the left renal vein and NOW the May thurner syndrome!
Just like the renal, one notes decreased contrast at the lower arrow where common iliac artery crosses over the iliac vein. And as mentioned before, note the very large and prominent Ascending Lumbar Vein (upper arrow and ALV).
So we have a compromised cerebrospinal circulation with the added venous flow of the left renal vein and the left leg. Treatment of both these veins seems compelling to relieve the CCSVI.
But i did not do it at this stage. Why? My logic says that added flow through the azygous vein may actually be beneficial during the recovery from the azygous stenting and reduce the short term risk of thrombosis.
Also the patient was kind of overwhelmed by the prospect of two stents.
Angioplasty alone of these compression syndromes is not particularly effective since the compressive effect is not overcome long term by angioplasty. Stents provide the buttress to hold open the vein.
So to summarize:
1. An inexperienced interventionalist underestimated the significance of the left internal jugular stenosis and did no t treat it.
2. A valvular stenosis of the azygous vein was unrecognized by venography but very well visualized by IVUS.
3. A Stenosis of the ascending part of the azygous vein was resistant to angioplasty and required a stent.
4. a stenosis of the J3 segment of the left internal jugular vein was postural in nature. Whether treatment will be necessary depends upon the patient's degree of improvements from the conventional treatment.
5. May thurner sydrome and Nutcracker syndrome are compression syndromes that require stenting. I think i took an interesting approach to utilize this increased flow to improve chances of avoiding thrombosis of the azygous stenting.
6. I have introduced you to another IR procedure as part of the planning of the CCSVI procedure. UFE has been shown through quality of life studies to improve quality of life from symptomatic uterine fibroids with low risk. A recent randomized prospective trial with long term followup showed, unexpectedly, that UFE has superiority over hysterectomy for this.
That is all for today, class. Have a great evening.