Page 366 of 557
Posted: Sun Jul 24, 2011 11:36 am
by Cece
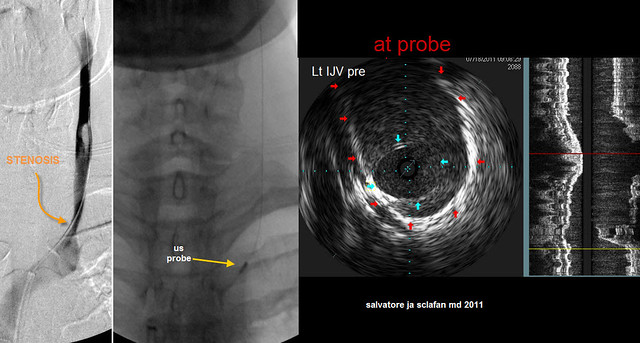
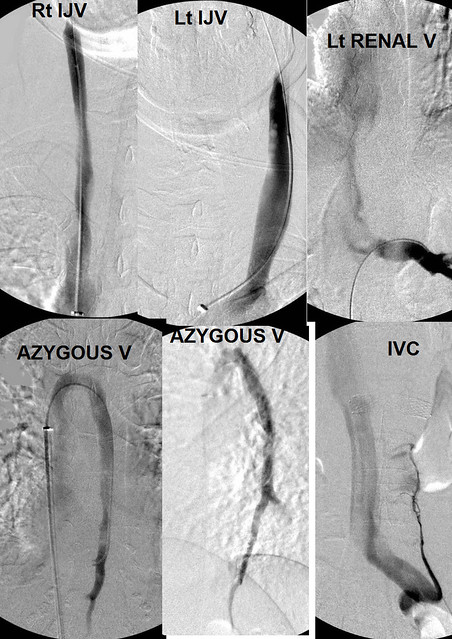
drsclafani wrote:LEFT JUGULAR VEIN
The rest of the IJV was also a challenge. Flow was slow and collaterals were visible. There was a slight narrowing of the lower end of the vein over a couple of centimeters
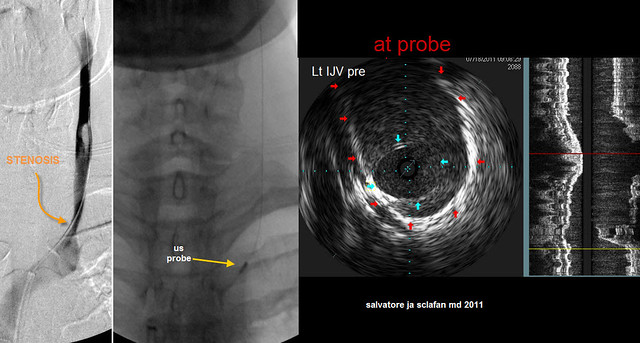
On the left image, there is a mild looking stenosis (curved orange arrow) that looks rather subtle. to the right of this a yellow arrow points to the ultrasound probe. The right of that is an IVUS image at the probe. The blue arrows point to the edges of a stenotic valve. The lumen of the valvular area is quite small compared to the full diameter of the vein (red arrows outline it). I estimate the narrowing to be at least 75%. It is clear that the IVUS does a better job of evaluating the stenosis and illustrating the pathology.
When you say it is mild-looking when seen under flouroscopy, what percentage would you estimate that as being, if that were the only imaging you'd had? Would you still have considered it significant enough to treat?
Posted: Sun Jul 24, 2011 11:43 am
by wonky1
Dear Dr Sclafani
Thank you for your prompt reply.
I last had images, a venogram, done when I had my last jugular stent in March of 2010.
I do not know if there is any intimal hyperplasia. My last stent placement
hurt like I'd been kicked by a horse though and an ultrasound done last year showed my jugulars were thickened, so I surmise there is.
Whilst I do not regret jumping into this as it offered hope where previously there was none, in retrospect it would have been better to wait until more was known and IVUS was available. I hope that by being such an "early adopter" I have not ruined my chances of further/renewed improvement.
Posted: Sun Jul 24, 2011 11:49 am
by Cece
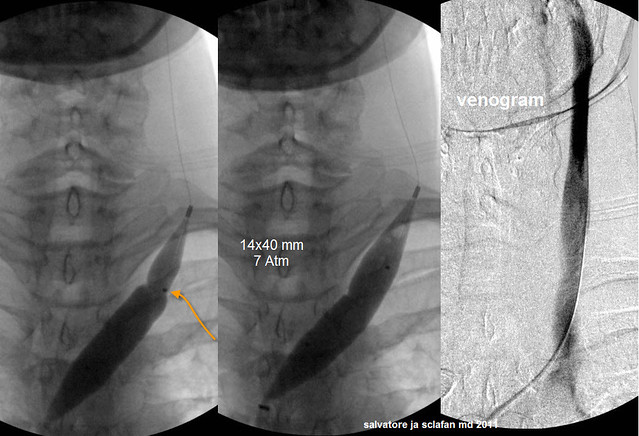
drsclafani wrote:TREATMENT OF LOWER LEFT INTERNAL JUGULAR STENOSIS
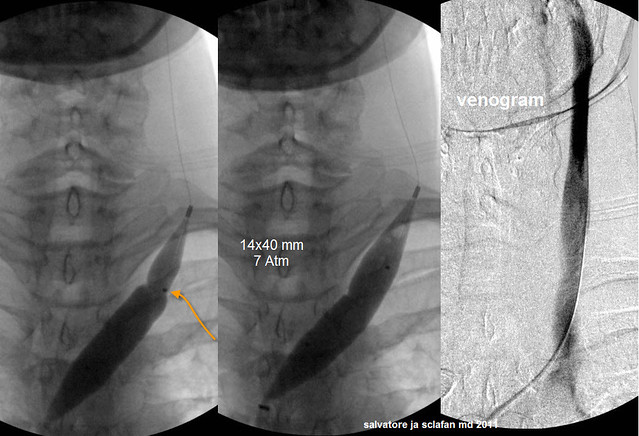
This valvular stenosis was treated with a 14 millimeter balloon which, when inflated, has a surface area about 50% greater than the full vein wall. Since the vein is larger below the stenotic valve, the balloon is positioned eccentrically with the majority of the balloon below the valve. This prevents stretching the normal vein. At 7 atmospheres the waist on the balloon was eradicated and there was no elastic recoil noted.
The image on the right shows improved diameter and improved faster flow.
We sometimes see perfectly smooth balloons when the waisting gives way and we sometimes see a little indent still. I can see a little indent in this one and also in my own:
www.thisisms.com/ftopicp-171131.html#171131
Even if there is still an indent, is it no longer considered to have waisting? I can see in today's example how much it gave way on the other side.
Posted: Sun Jul 24, 2011 12:04 pm
by wonky1
Dear Dr Sclafani
Thank you for your prompt reply.
I last had images, a venogram, done when I had my last jugular stent in March of 2010.
I do not know if there is any intimal hyperplasia. My last stent placement
hurt like I'd been kicked by a horse though and an ultrasound done last year showed my jugulars were thickened, so I surmise there is.
Whilst I do not regret jumping into this as it offered hope where previously there was none, in retrospect it would have been better to wait until more was known and IVUS was available. I hope that by being such an "early adopter" I have not ruined my chances of further/renewed improvement.
Although I have stents now they were done after ballooning had failed.
Pity they are stainless steel as although I have been assured they are MRI safe I understand that they will cause artefacts ruining the image.
Posted: Sun Jul 24, 2011 12:19 pm
by Cece
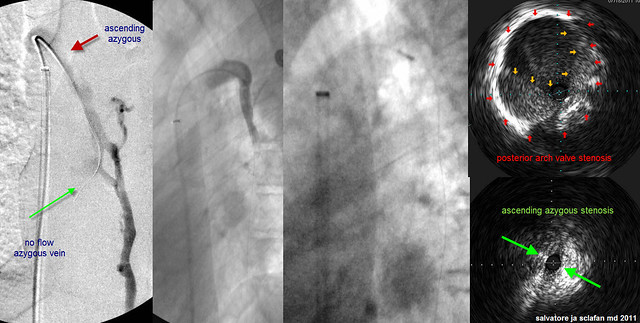
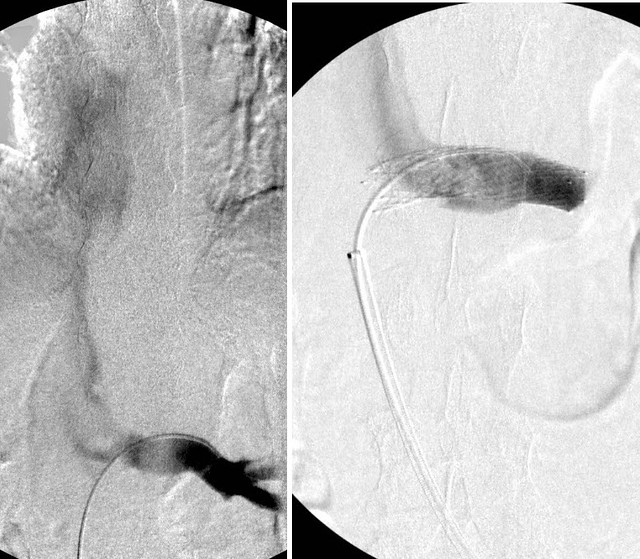
drsclafani wrote:AZYGOUS VEIN
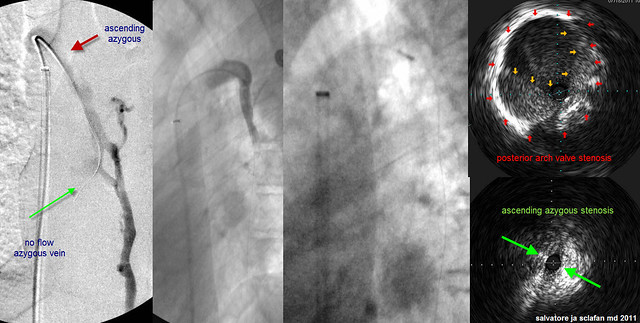
The left image shows the azygous vein in the frontal view. Notice how one cannot really evaluate the arch of the azygous which is m uch better seen in a steep oblique of "off" lateral. There is reflux in the hemiazygous vein but there is no flow down the azygous vein (green arrow). Other collateral veins are also seen. The upper portion of the ascending azygous vein (red arrow) is poorly seen and likely there is obstruction there.
This is a unique azygous vein from the others we have seen. I can't remember being shown one where there is no flow like this.
Would the stenosis in the ascending azygous be considered a hypoplasia?
Angioplasty had NO effect on this stenosis and there was still no flow. So a stent was placed in order to get some flow. I would prefer not to use stents but failure of repeated angioplasty to open up a vein is one of my indication to stent. Followup venography (far right) shows improved flow.
It is amazing to see the flow restored.
I bet Nutcracker syndrome. Does treatment of this syndrome improve symptoms of ccsvi? I will review soon another patient who had already been treated for CCSVI (BUT NOT NUTCRACKER) who has already shown improvements of the prior CCSVI treatment.
So such a patient might help tease out the effects of treating for Nutcracker?
You have a backlog of interesting cases to share!
This is a perfect storm, not only left jugular and azygous stenoses but compressions of BOTH the left renal vein and NOW the May thurner syndrome!
A perfect storm indeed....
Your patient has my best wishes for improved health and well-being.
Posted: Sun Jul 24, 2011 3:10 pm
by drsclafani
Cece wrote:drsclafani wrote:5. May thurner sydrome and Nutcracker syndrome are compression syndromes that require stenting. I think i took an interesting approach to utilize this increased flow to improve chances of avoiding thrombosis of the azygous stenting.
Once the azygous has healed and the stent endothelized, would you recommend this patient receive treatment for the two compression syndromes?
absolutely!!!!
i deferred the treatment of these two compressions with the understanding that we would come back and revisit this.
i think that there is a real opportunity there.
Posted: Sun Jul 24, 2011 3:14 pm
by drsclafani
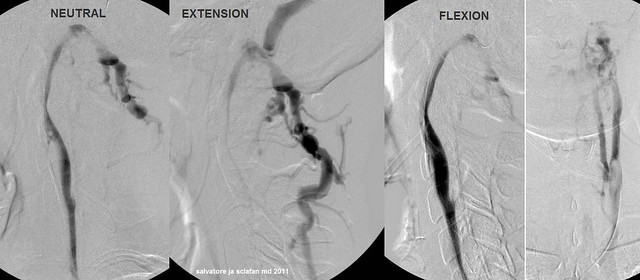
Cece wrote:drsclafani wrote:vein is imaged in a neutral, a flexion and an extension position.
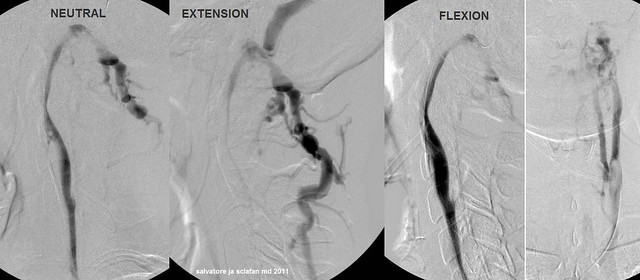
As you can see, the narrowing is related to position of the neck. When in the neutral position it is compressed. When the neck is placed in full extension, the narrowing is greater and the collaterals are larger. it is interesting to see that flexion of the neck leads to reduction in the compression, improvement in flow and reduction of vertebral collateralization.
What will ultimately be recommended for such lesions is unclear at this time. On the first treatment, I decided NOT to treat by angioplasty or stenting. We will see how this patient does with standard treatments and then decide what to do about this in the future as we see how she responds.
So discussion number one. Should I have stented this vein?
Tough call.
Pros would be the opportunity to normalize flow in the vein, independent of posture.
Cons would be risk of accessory spinal nerve damage, complications of the stent such as intimal hyperplasia, thrombus, etc, with potential compromise of the vein, potential damage to the stent because of compression against the spine, and the fact that if left alone the vein will still have flow in at least some positionings.
After reviewing the entire case, this patient had so many issues, there is the potential to benefit from the treatment of the other areas, even if this area has gone untreated. It might have been more tempting to treat this upper area if it had been the only abnormality found.
One question: do you think leaving this upper area untreated will mean lesser flow and thereby negatively affect the healing of the lower area in the jugular that was treated?
i think that this problem needs to be corrected by better sleeping devices, perhaps improved pillows and re-education about positions of sleep....easier said than done. We must also understand that the position of the head for the procedure is not natural, only reproducible. Tilting the head only a little bit made a difference in flow and reflux.
not easy decisions but certainly not the first decisions to make
Posted: Sun Jul 24, 2011 3:23 pm
by drsclafani
wonky1 wrote:Dear Dr Sclafani
Thank you for your prompt reply.
I last had images, a venogram, done when I had my last jugular stent in March of 2010.
I do not know if there is any intimal hyperplasia. My last stent placement
hurt like I'd been kicked by a horse though and an ultrasound done last year showed my jugulars were thickened, so I surmise there is.
Whilst I do not regret jumping into this as it offered hope where previously there was none, in retrospect it would have been better to wait until more was known and IVUS was available. I hope that by being such an "early adopter" I have not ruined my chances of further/renewed improvement.
it sounds like there might have been a mis-sizing of the stent. too large a stent stretches the adventia which is where pain fibers are located. That constant stretching of the vein because the stent is too large may be responsible for the intimal hyperplasia you speak about.
the retrospectoscope is a pain in the rear. I meant no criticisms of you or your doctor.
your days of pioneering are not yet completed
s
Posted: Sun Jul 24, 2011 3:25 pm
by drsclafani
Cece wrote:drsclafani wrote:TREATMENT OF LOWER LEFT INTERNAL JUGULAR STENOSIS
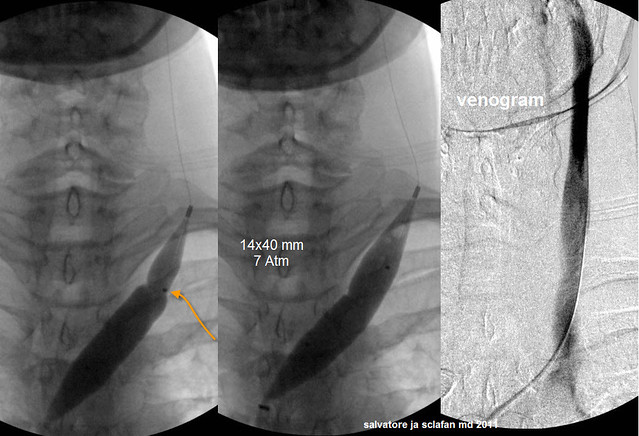
This valvular stenosis was treated with a 14 millimeter balloon which, when inflated, has a surface area about 50% greater than the full vein wall. Since the vein is larger below the stenotic valve, the balloon is positioned eccentrically with the majority of the balloon below the valve. This prevents stretching the normal vein. At 7 atmospheres the waist on the balloon was eradicated and there was no elastic recoil noted.
The image on the right shows improved diameter and improved faster flow.
We sometimes see perfectly smooth balloons when the waisting gives way and we sometimes see a little indent still. I can see a little indent in this one and also in my own:
www.thisisms.com/ftopicp-171131.html#171131
Even if there is still an indent, is it no longer considered to have waisting? I can see in today's example how much it gave way on the other side.
good observation cece, one I expected you to mention.
if the balloon were fully inflated, that waist would be gone. When the balloon is on a curve, there tends to be a crease in the balloon at the apex of that curve. That was the case here. This was the best image I had
Posted: Sun Jul 24, 2011 4:03 pm
by magoo
NZer1 wrote:Hi everyone, I have a question for you all.
Has anyone who has been retreated gained more improvements on the later treatments than on the first?
I have not seen in my recall anyone who has been retreated that has had new or better improvements as though the first treatment has been the benchmark for the symptom changes and it is in my understanding we don't know if there is a halt in progression.
Can anyone say that they have had a halt in progression at this time?
Nigel,
My improvements were great after the first treatment. I had my second because of a return of headaches, heat intolerance, and a few other things. I was under treated the first time because it was very early. The second has certainly proven to be more beneficial. I am not 100%, and I feel some damage is permanent, but I am not progressing. My recent MRI was stable!
Posted: Sun Jul 24, 2011 4:26 pm
by Cece
So to summarize:
1. An inexperienced interventionalist underestimated the significance of the left internal jugular stenosis and did no t treat it.
At least the newbie IR did no harm. We've seen worse.
2. A valvular stenosis of the azygous vein was unrecognized by venography but very well visualized by IVUS.
Another coup d'IVUS.
3. A Stenosis of the ascending part of the azygous vein was resistant to angioplasty and required a stent.
Stenosis of the ascending azygous is rare, isn't it? How often do you see it, on estimate?
Did you see my find of an azygous-to-iliac image?
www.thisisms.com/ftopicp-171537.html#171537
Pretty neat, yes?
4. a stenosis of the J3 segment of the left internal jugular vein was postural in nature. Whether treatment will be necessary depends upon the patient's degree of improvements from the conventional treatment.
5. May thurner sydrome and Nutcracker syndrome are compression syndromes that require stenting. I think i took an interesting approach to utilize this increased flow to improve chances of avoiding thrombosis of the azygous stenting.
I understand the reasoning here. It's clever.
6. I have introduced you to another IR procedure as part of the planning of the CCSVI procedure. UFE has been shown through quality of life studies to improve quality of life from symptomatic uterine fibroids with low risk. A recent randomized prospective trial with long term followup showed, unexpectedly, that UFE has superiority over hysterectomy for this.
That is all for today, class. Have a great evening.
You have a great evening too, professor....
Posted: Sun Jul 24, 2011 4:30 pm
by Cece
drsclafani wrote:Cece wrote:drsclafani wrote:TREATMENT OF LOWER LEFT INTERNAL JUGULAR STENOSIS
This valvular stenosis was treated with a 14 millimeter balloon which, when inflated, has a surface area about 50% greater than the full vein wall. Since the vein is larger below the stenotic valve, the balloon is positioned eccentrically with the majority of the balloon below the valve. This prevents stretching the normal vein. At 7 atmospheres the waist on the balloon was eradicated and there was no elastic recoil noted.
The image on the right shows improved diameter and improved faster flow.
We sometimes see perfectly smooth balloons when the waisting gives way and we sometimes see a little indent still. I can see a little indent in this one and also in my own:
www.thisisms.com/ftopicp-171131.html#171131
Even if there is still an indent, is it no longer considered to have waisting? I can see in today's example how much it gave way on the other side.
good observation cece, one I expected you to mention.
if the balloon were fully inflated, that waist would be gone. When the balloon is on a curve, there tends to be a crease in the balloon at the apex of that curve. That was the case here. This was the best image I had
ohhhh
did not know that.
Posted: Sun Jul 24, 2011 4:30 pm
by drsclafani
NZer1 wrote:Hi everyone, I have a question for you all.
Has anyone who has been retreated gained more improvements on the later treatments than on the first?
I have not seen in my recall anyone who has been retreated that has had new or better improvements as though the first treatment has been the benchmark for the symptom changes and it is in my understanding we don't know if there is a halt in progression.
Can anyone say that they have had a halt in progression at this time?
nigel, if you read the first case i presented today, you will see a patient who was not treated on the first go around who had angioplasty of the left IJV and two lesions in the azygous treated by angioplasty and stenting respectively. I did not treat a nutcracker syndrome of the left kidney.
if i might be so bold as to share another case in which the patient had treatment the first time in India with some improvements that lasted a few months and then recurred. I treated her this past week.
From the angiogram you can see that the treated right and left IJV were is good shape and the azygous vein that was not treated remains normal.
in this caase i treated a nutcracker syndrome as the only treatment in the second procedure.
Here are the diagnostic venograms:
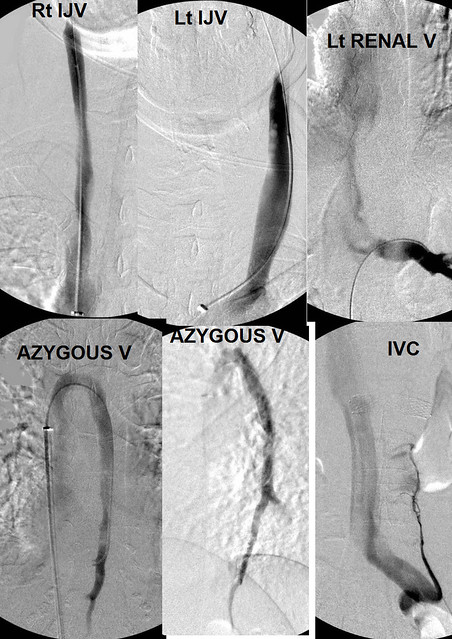
Both internal jugular veins were of normal caliber as was the azygous vein. There is an indentation on the renal vein.
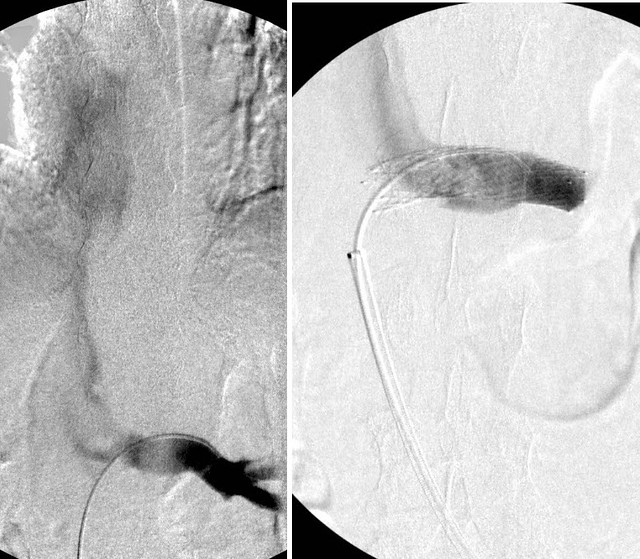
A stent was placed and flow is normal now
i attach the patient's report to me:
Hi Dr. Sclafani
Thank you and your team for your excellent care on Monday, and for such an informative and inspiring session on friday.
I know I'm not due to give you an update until Aug. 18th but thought I would give you a quick 5 day update. I am doing well. I think my situation is unique because I assume that whatever benefits I receive this time around can be attributed to the stent in my renal vein and the resulting improved blood flow rather than ballooning of the jugulars or azygous, or any valve work. And I have had a few improvements over and above the improvements I had the first time.
On day 2, I noticed an improvement in my vision while driving in the taxi. I have a greater sense of depth, everything is clearer and colours are brighter. I'm so pleased to have a second improvement. After my first angioplasty it took a month before I noticed improved vision and I thought that I had kept the improvement for the past year. However, I now realize that I had lost some of my benefits and my vision is now top notch again. This is especially pleasing to me because we have just completed our retirement home with a beautiful view over the Ottawa River.
My balance has improved further. I just completed 38 steps heel to toe and stopped only because I ran out of hallway. While my balance improved considerably the first time I couldn't do more than about 7 or 8 steps without loosing my balance. I feel that my gait is also slightly improved. However, I still have the constant pain and fatigue in my legs. I am hopeful I will see further improvement in my ability to stand and walk but am mindful that my lumbar veins are not normal.
I am still periodically tired and drained from the procedure--I slept much of the first 24 hours. My torso, lower abdomen and lower back were sore for about 3 days (and are occasionally tender) and the wound bled a little bit until thursday but aside from a large bruise it seems fine now. I seem to be tolerating the pradaxa and aspirin well.
I'm wondering how many patients you have found with nutcracker syndrome and how many with May Thurners syndrome since you started looking at the renal and iliiac veins? From what I have read online it seems that nutcracker syndrome is quite rare (although perhaps it is just underdiagnosed) yet you found it in 2 patients in one day. Is this congenital or did I develop it sometime over my lifetime? Perhaps the name CCSVI should be changed to chronic venous insufficiency?
Bottom line--I'm very glad I had a second procedure, and of course am even happier with my choice of Dr. I will be in touch again on Aug. 18th
Take care and I will continue to follow you on TIMS. Thanks again,
This is a really interesting and unique test of the effect that renal vein stenosis can have on symptoms of CCSVI since no other treatment was performed and rather dramatic changes occured.
Posted: Sun Jul 24, 2011 4:47 pm
by Cece
Stent the renal vein, and vision and balance improves!!
We are such odd patients.
It surprises me that some doctors would diagnose MT or renal vein stenosis and treat by ballooning. And of course there was the earlier suggestion that it was wrong to be looking for these compression syndromes in asymptomatic patients. But here is another happy patient who has had this treated and we learn something, based on her immediate improvements, about the impact of these seemingly unrelated veins on our cerebrospinal drainage.
Well done....
Posted: Mon Jul 25, 2011 5:24 am
by HappyPoet
drsclafani wrote:i think that this problem needs to be corrected by better sleeping devices, perhaps improved pillows and re-education about positions of sleep....easier said than done. We must also understand that the position of the head for the procedure is not natural, only reproducible. Tilting the head only a little bit made a difference in flow and reflux.
Thanks, DrS, for putting this case together. I can't believe how much I keep learning from you.
In what way(s) can pillows be improved?
Regarding "re-education about positions of sleep," what sleep positions do you recommend?
Thank you!