MikeInFlorida wrote:Dear Dr. Sclafani,
I have a thousand questions, but I'm not sure how to start, so I'll start by "blurting" a few (probably unimportant questions) while I collect my thoughts.
Hi, mike....how is our mutual friend doing
1. Why did you start with the right instead of the left (this is pure curiosity)?
I go where the catheter takes me. Sometimes its left, sometimes its right. No more intelligent answer than that.
2. Why did you try for 15 minutes on the right, then for 45 minutes (or more if it had taken more) on the left?
actually 40 min on right and 20 min on the left...glad i made that clear from the beginning.

Were you expecting one of the two IJV's to be easier than the other? I guess I'm asking, is it unusual for both IJV's to be such a PITA (pain in the a$$)?
i have learned to expect nothing, but hope for simple anatomy and cooperative orifices.
3. The emissary vein collateral... my anatomy book doesn't show it traversing the hypoglossal canal. The only pic I can find of the emissary vein is superior to the saggital sinus (Netter Atlas, plate 99 and 101).
Look for images of the cranial canals. anything that can transmit a nerve can have a vein travel along,
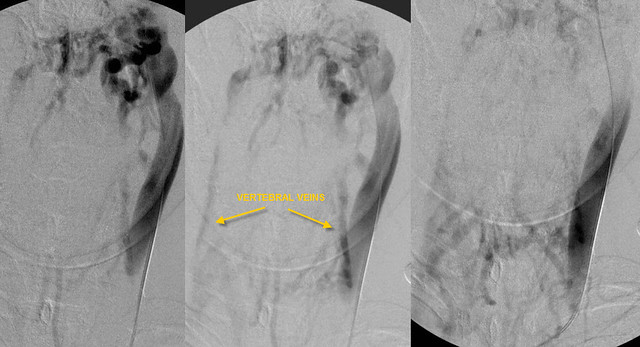
the following emissary veins are mentioned
mastoid emissary vein
thru mastoid foramen: transverse sinus to posterior auricular or occipital vein
parietal emissary v
thru parietal foramen: superior sagittal sinus to scalp veins
rete canalis hypoglossi
thru hypoglossal canal: transverse sinus to vertebral v and deep cervical veins
condyloid emissary vein
thru condyloid canal transverse sinus to deep veins of the neck
rete foraminis ovalis
thru foramen ovale cavernous sinus to pterygoid plexus
emissary vein of foramen of Vesalius and foramen lacerum
cavernous sinus to pterygoid plexus
internal carotid plexus
thru the carotid canal: cavernous sinus to IJV
Superior sagittal sinus with the veins of the nasal cavity.
4. How could the contrast dye possibly illuminate the right IJV? A previous commenter hypothesised that the right IJV does not exist because it was not illuminated by the refluxed dye injected into the left IJV. Do the right and left IJV's communicate throught the emissary veins?
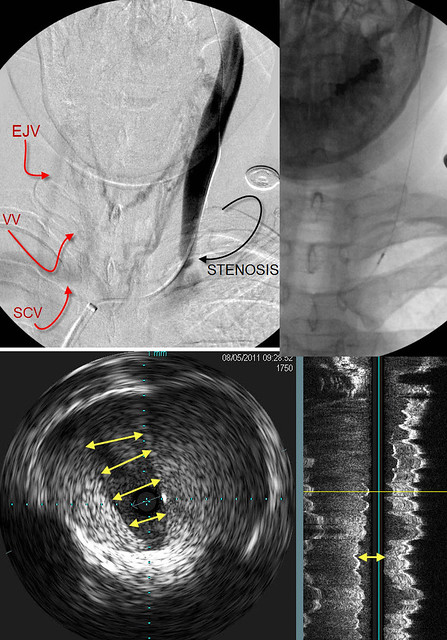
the emissary veins connect the dural sinuses to the extracranial veins by emissary veins that travel through the bony skull
5. I was about to hit the "submit" button, but saw the "mastoid emissary" in the general vicinity of the jugular bulb (the condylar emissary vein is also nearby). If either of these are the referenced collateral, please ignore #3 (but which one?). If not, please explain my confusion.
please share my confusion
6. How much radiation is the patient exposed to during a nominal procedure?
7. How much are you and your staff exposed to radiation during a nominal procedure?
i am getting actual numbers for all my cases. this will take a while.
These are random, simple (blurted) questions. I am fascinated by this case, and I hope to have more and better questions soon. I look very much forward to hearing more about this.
Mike
I am sure you do