Page 1 of 7
plethysmography neck collars (Zamboni)
Posted: Thu Nov 25, 2010 8:55 pm
by Cece
[Dr. Zamboni] is conducting a new round of tests in which subjects will wear a collar fitted with a strain gauge to measure neck volume differences in the upright and prone positions. This will allow him to measure the time it takes for for blood to drain through the neck in MS vs. control subjects. This technique is called plethysmography and is less operator-dependent than Doppler ultrasound.
http://www.acceleratedcure.org:8080/node/3605
Re: plethysmography neck collars (Zamboni)
Posted: Fri Nov 26, 2010 2:15 am
by frodo
Cece wrote:[Dr. Zamboni] is conducting a new round of tests in which subjects will wear a collar fitted with a strain gauge to measure neck volume differences in the upright and prone positions. This will allow him to measure the time it takes for for blood to drain through the neck in MS vs. control subjects. This technique is called plethysmography and is less operator-dependent than Doppler ultrasound.
http://www.acceleratedcure.org:8080/node/3605
How do you find always the best articles?
Thanks anyway.
Posted: Fri Nov 26, 2010 2:15 pm
by Cece
Thanks, frodo. I would've thought this was a joke (neck collars, really?) but it's from Dr. Zamboni.
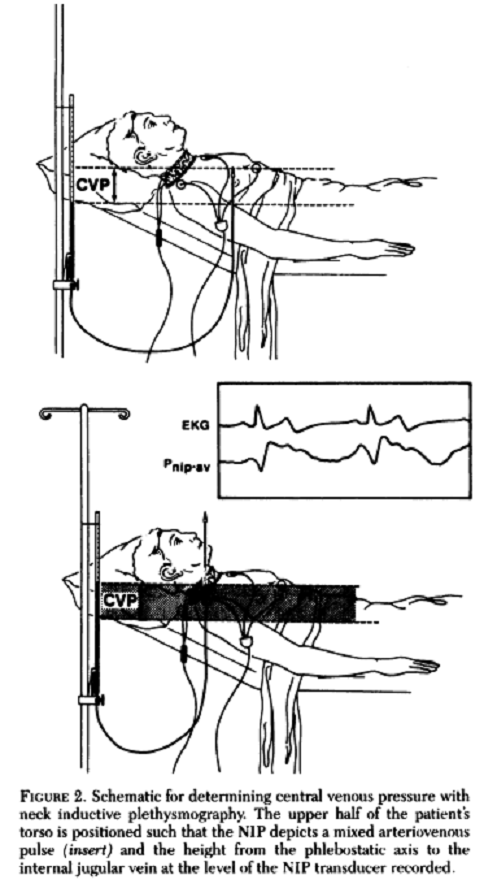
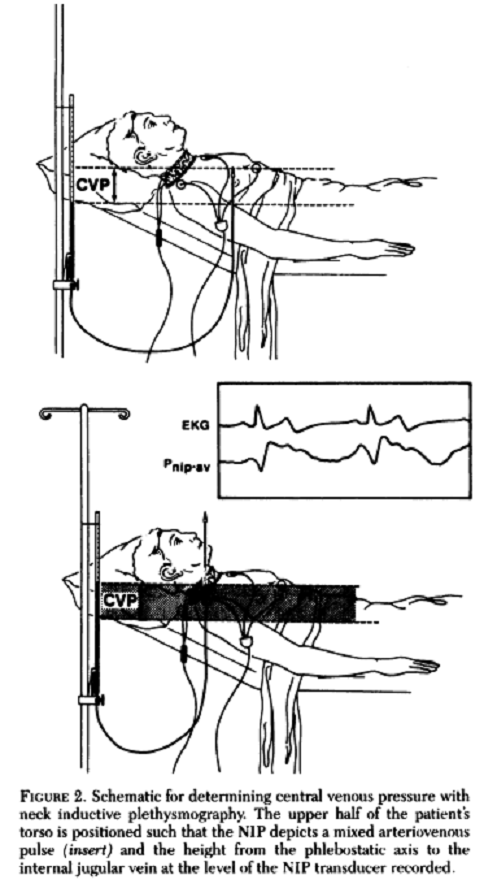
I dug up an article on plethysmography with diagrams of what the neck collar looks like.
Chest. 1991 Aug;100(2):371-5.
Noninvasive measurement of central venous pressure by neck inductive plethysmography.
Bloch KE, Krieger BP, Sackner MA.
Division of Pulmonary Disease, University of Miami School of Medicine, Mount Sinai Medical Center, Miami Beach.
Abstract
Bedside estimation of the height at which the internal jugular veins collapse, referenced to a standard hemodynamic location, theoretically reflects central venous pressure. This method has never been demonstrated as accurate when compared to invasive CVP measurements because of the great clinical skills and time required to visually identify the internal jugular venous waveform. Since the principles of the bedside method are sound, we utilized them in conjunction with the neck inductive plethysmograph, a device which has the capability of recording internal jugular venous and carotid arterial waveforms. The respiratory distortion of these vascular waveforms was eliminated by employing a digital bandpass filter, making it easy to identify the venous and arterial waveforms on the videoscreen of a personal computer. The upper torso was positioned while observing the videoscreen until the vascular waveform was seen as a mixed arteriovenous waveform, signifying intermittent internal jugular venous collapse. The height of the internal jugular vein above the phlebostatic axis was obtained by external measurement and recorded as CVPni in cm H2O. In 43 patients, 86 percent of CVPni (NIP) values fell within 20 percent CVPi (invasive catheter measurements) over a range of CVP from 0 to 19 cm H2O. In an additional seven patients, CVPi was greater than the height that the upper torso could be elevated and an arterial waveform could not be obtained. Here, CVPni was recorded as the value at least exceeding the value measured. In two other patients, obstruction of an internal jugular vein gave spuriously low values of CVPni. Our study indicates that this new neck inductive plethysmographic method is accurate compared to invasive catheter measurements of CVP and should serve as a safe, noninvasive alternative in situations where such measurements are required.
Full article and diagrams here:
http://chestjournal.chestpubs.org/conte ... 1.full.pdf
For the two with IJV occlusions, one had an indwelling cathether. When it was removed three days later, they measured the values again and they'd gone from abnormal to normal. The other was found to have a partial thrombosis and distended IJV. They measured again after the veins were patent. It's in the last paragraph on page 373 of the article.
What I'm taking from it is that for our exact situation (IJV occlusions when it's pre-venoplasty and occlusion-free IJVs when it's post-venoplasty) the plethysmography shows a measurable difference.
Posted: Sat Nov 27, 2010 1:34 pm
by CuriousRobot
If CVPi is greatly elevated, then the maximal upright
distance between the neck and the phlebostatic axis
may be insufficient to achieve collapse of the internal
jugular veins. This occurred in three patients with a
small vertical torso related to kyphoscoliosis, in three
patients in whom recent abdominal surgery prevented
full upright positioning, and in one patient who had
extreme orthostatic hypotension. Nevertheless, in all
these patients, despite this limitation, CVPni revealed
elevated values above the upper limit of normal of 7
cm H2O.’#{176}
When Zamboni said, "it's the posture," or something like that, he really wasn't kidding.
Posted: Tue Mar 15, 2011 2:19 pm
by Cece
This fits with the discussion of plethysmography at ISNVD today.

Posted: Tue Mar 15, 2011 3:20 pm
by cheerleader
This is such a brilliant discovery by Dr. Zamboni, and a wonderful use of current technology...but I can't help thinking it was inspired by the letter he wrote in response to the Doepp study. Remember? He said that the extra blood volume noted by the neurologists in pwMS in the neck in the upright position was actually PROOF of CCSVI? Due to extracranial blockage. And now, he's shown just that with the study of 100 people (50 normals/50 pwMS) using this collar.
incredibly exciting. Good job getting the pics and research on this thread, Cece!
cheer
Posted: Tue Mar 15, 2011 5:17 pm
by msscooter
Thanks for bringing us this important report. This test should be easy to reproduce and help open the gates to the IR kingdom.
I've been so curious by posture. always troubled by it, and now as a liberati wonder what posture is optimal for my problem. awake, at the computer and asleep.
Posted: Tue Mar 15, 2011 6:30 pm
by Athena
msscooter,
I was thinking the same thing last night. What postures are good and not good for me in relation to venous return from my brain and spinal cord.
Kind regards,
Athena
Posted: Tue Mar 15, 2011 6:45 pm
by Cece
If you notice the date on the original post, it's been since November that I've been waiting for Zamboni to spill the beans on plethysmography! Today was excellent. Is there more information about the 50/50 patient study? And yes, what he said to the Doepp response may mean either he was already thinking about blood volume in the neck or he was inspired right then. What a brilliant man.
Posted: Wed Mar 16, 2011 12:21 am
by ikulo
Doesn't this contraption measure venous pressure and not flow? Wasn't there a debate here before about CCSVI being about flow and not pressure?? Someone explain this to me, I'm feeling denser than usual.

Posted: Wed Mar 16, 2011 12:51 am
by hh
Great report and additional information. Somehow I can't believe wev aren't needing to also think of the Haacke protocol and the great benefits he is able to show with his MR Imaging knowledge and technique. His MRI reports are also invaluable to science and the patient giving hard data that patients can hold onto for both first and ongoing treatment. The data is extremely revealing and proficient (for lack of better word) to science. We cannot forget the importance of a more detailed data on our veins. More soon again. Tired. It's now 1:50 AM.
Posted: Wed Mar 16, 2011 6:42 am
by cheerleader
ikulo wrote:Doesn't this contraption measure venous pressure and not flow? Wasn't there a debate here before about CCSVI being about flow and not pressure?? Someone explain this to me, I'm feeling denser than usual.

Good point, ikulo. You are far from dense. I believe Dr. Zamboni had his "a ha" moment while writing up his response to the Doepp study. If you remember, the only abnormality that study found was the amount of blood in the veins changed more in normals then pwMS when going from supine to upright. Here's Dr. Zamboni's response (which has no abstract online by the Annals of Neurology (what a surprise!) but I got a copy of the whole letter)
One of the major regulators of cerebral venous outflow is posture, due to the gravitational gradient between the cerebral parenchymal veins and the base of the neck (␣30mmHg).2 The authors demonstrate a much larger change in blood flow volume in normal subjects compared to MS patients when the subjects go from a supine to an upright position. They find a change of 128ml/min and 56ml/min for the right and left sides, respectively, for MS patients. But they find a much larger change of 266ml/min and 105ml/min for their normal subjects. This result actually suggests the presence of chronic cerebrospinal venous insufficiency (CCSVI). Possible causes include intra-luminal septum, membrane, and immobile valve affecting the hydrostatic pressure gradient in the upright position. The presence of such blockages in the extracranial and extravertebral cerebral veins has been proven also by using catheter venography, the unquestionable gold standard in medicine.3,4
So, the collar can point to this lack of change in pwMS, and change in normals....which is exactly what it did in Zamboni's collar study (paper to follow) This is an idiot proof way to show that there's something wrong....not neuros waving doppler wands around saying there's nothing there...just a collar, and a readout. It is cost-efficient and operator independent, just like a blood pressure cuff which tells many they have a heart condition that needs to be addressed. It does not show location of the blockage (you will need doppler/venography for that) BUT it shows the problem.
If blood stays in the neck, and does not return to the heart in a timely manner, you have a health issue. Thanks to the Doepp study for making that clear.
cheer
Posted: Wed Mar 16, 2011 6:45 am
by Cece
ikulo wrote:Doesn't this contraption measure venous pressure and not flow? Wasn't there a debate here before about CCSVI being about flow and not pressure?? Someone explain this to me, I'm feeling denser than usual.

I am not sure about the pressure measurement either. My understanding is that Dr. Zamboni is using this neck collar to measure volume in the neck. Volume in the neck would be an indirect measurement of outflow obstructions, because those obstructions would increase the congestion which would increase the volume.
Do any of our IRs or their hospitals have a neck plethysmography set-up?
I wonder what the sensitivity of the plethysmography is, if it can measure differences even if there is only one jugular with an obstruction and the other one is fully functional.
I wonder if there is a use for it in measuring venous congestion in patients with unilateral ligation. I posted the other day about children getting jugular ligation as a treatment for jugular phlebectasia. There are also plenty of reports of surgeons removing a jugular as a graft to use for a problem elsewhere. It needs to get into the medical literature that ligation or removal of the jugular has more possible consequences than previously thought. Even before we are all helped, there is a need for the doctors to stop doing harm unknowingly.
Whew, Cheer has answered the question while I've been working on this post. That's a tough question Ikulo.

Posted: Wed Mar 16, 2011 6:47 am
by cheerleader
hh wrote:Great report and additional information. Somehow I can't believe wev aren't needing to also think of the Haacke protocol and the great benefits he is able to show with his MR Imaging knowledge and technique. His MRI reports are also invaluable to science and the patient giving hard data that patients can hold onto for both first and ongoing treatment. The data is extremely revealing and proficient (for lack of better word) to science. We cannot forget the importance of a more detailed data on our veins. More soon again. Tired. It's now 1:50 AM.
I agree 100%, HH--the problem is that not all have access or $ to do the Haacke protocol. It is time intensive, expensive and involves follow-up commitment. It is giving more to science and the understanding of CCSVI-- how angioplasty changes the brain, and the damage that CCSVI can create. Those who are participating are doing a great thing for science (and themselves) but it will not be available in third world nations (or even Canada....) A pressure cuff is less expensive, less difficult to mess up, and will get more people diagnosed faster...and that is a good thing, too.
cheer
Posted: Wed Mar 16, 2011 6:54 am
by Rokkit
cheerleader wrote:If blood stays in the neck, and does not return to the heart in a timely manner, you have a health issue. Thanks to the Doepp study for making that clear.