Page 2 of 7
Posted: Thu Jan 13, 2011 9:24 am
by DrCumming
Sal, I think the left IJ maybe occluded at the skull base. I do not see the sigmoid sinus filling.
On that note, I saw a patient treated in Mexico. Imaging was on an ancient 512k cardiac room (no DSA). They ballooned the proximal IJ without looking at the distal IJ. She did not improve. When I imaged here, we found a complete occlusion of the distal IJ at the skull base. Crossed and ballooned that. Modest symptom improvement.
Re: CASE STUDY #1
Posted: Thu Jan 13, 2011 10:22 am
by drsclafani
uprightdoc wrote:drsclafani wrote:uprightdoc wrote:
we strongly disagree about whether any inferences can be made about spinal curvature on these images.
Posted: Thu Jan 13, 2011 10:24 am
by drsclafani
DrCumming wrote:Sal, I think the left IJ maybe occluded at the skull base. I do not see the sigmoid sinus filling.
On that note, I saw a patient treated in Mexico. Imaging was on an ancient 512k cardiac room (no DSA). They ballooned the proximal IJ without looking at the distal IJ. She did not improve. When I imaged here, we found a complete occlusion of the distal IJ at the skull base. Crossed and ballooned that. Modest symptom improvement.
which vein is the IJV? WHAT IS ITS COURSE.
I spent more than 30 minutes trying to get into the LIJV. When i catheterized the branch on the left #1, i expected that it was NOT the IJV. I was using it to find the IJV.Then we have this tangle of veins, left me moderately confused.
help me find my way

Re: CASE STUDY #1
Posted: Thu Jan 13, 2011 10:33 am
by drsclafani
uprightdoc wrote: at least we both agree that CCSVI plays a role in MS.
I won't give you that one either. I am not sure whether they are cause and effect, or just associations. I am not sure which symptoms are caused by MS and which symptoms are caused by CCSVI.
i am still awaiting data confirming dr zamboni's original paper that angioplasty is a durable effective treatment and i hope to come to my own very early conclusions in 2012.
And I hope to publish a 25 year review of long term outcomes of "Liberation" in 2035 at the ripe old age of 88
I remain my most passionate skeptical self

Posted: Thu Jan 13, 2011 10:39 am
by DrCumming
drsclafani wrote:DrCumming wrote:Sal, I think the left IJ maybe occluded at the skull base. I do not see the sigmoid sinus filling.
On that note, I saw a patient treated in Mexico. Imaging was on an ancient 512k cardiac room (no DSA). They ballooned the proximal IJ without looking at the distal IJ. She did not improve. When I imaged here, we found a complete occlusion of the distal IJ at the skull base. Crossed and ballooned that. Modest symptom improvement.
which vein is the IJV? WHAT IS ITS COURSE.
I spent more than 30 minutes trying to get into the LIJV. When i catheterized the branch on the left #1, i expected that it was NOT the IJV. I was using it to find the IJV.Then we have this tangle of veins, left me moderately confused.
help me find my way

ah there is the value of pre procedure imaging... you can use on table US to confirm you are in or not in the IJ. i have done that once or twice. also a more lateral view might be of value. if you are holding a gun to my head, i would choose the first 2 images as being the ijv

.
Re: CASE STUDY #1
Posted: Thu Jan 13, 2011 12:09 pm
by uprightdoc
drsclafani wrote:uprightdoc wrote: at least we both agree that CCSVI plays a role in MS.
I won't give you that one either. I am not sure whether they are cause and effect, or just associations. I am not sure which symptoms are caused by MS and which symptoms are caused by CCSVI.
Actually, MS doesn't cause signs and symptoms. MS is a merely a label for a condition associated with a constellation of signs and symptoms. In this regard there appears to be an association between venous drainage issues in the brain and MS signs and symptoms according to recent ccsvi research. Many of the symptoms of MS, however, sound suspicioulsly similar to vertebral-basilar artery insufficiency more than they do venous insufficency. In fact, both conditions may occur together as upper cervical misalignments can affect both the vertebral arteries and vertebral veins. What's more, if upper cervical misalignments can affect arterial and venous blood flow, then they most likely can affect CSF flow in the subarachnoid space as it returns from the cord and passes through the upper cervical spine on its way back to the superior sagittal sinus.
I began my research into the role of upright posture in neurodegenerative diseases in 1984 while studying artificially deformed and pathological crania, including hydrocephalus at the Museum of Natural History in NY. I also studied bats and giraffe skulls because of the extreme inversion flows they face, and I studied whale skulls because of the exposure to extreme Valsalva maneuvers. I published my first paper on the potential role of stenosis of the neural canal in neurodegenerative diseases in 1987. I am currently finishing the sequel to my first book, which deals more with arterial issues, and I am publishing a website based on my thirty years of investigation. I will be at it for over fifty years by the time I get to 88. Hopefully, sometime before then, we can get some research done on the biolgically highly plausible role of inherited and acquired disorders and degenerative conditions of the spine in neurodegenerative diseases. After all it wouldn't hurt to do some chiropractic research using Haake's protocols. It's very safe and inexpensive and it could benefit the patient. It may also help with prevention.
Re: CASE STUDY #1
Posted: Thu Jan 13, 2011 12:31 pm
by uprightdoc
drsclafani wrote:uprightdoc wrote:drsclafani wrote:
It's my opinion that plain view x-rays should be part of Haake's baseline studies. A basic visual orthopedic evaluation, however, or preferrably plumb line and scoliometer examination, or better yet a NUCCA anatometer, would indicate any tell-tale signs of curvature problems at the outset.
Re: CASE STUDY #1
Posted: Thu Jan 13, 2011 12:44 pm
by phlebologist
drsclafani wrote:phlebologist wrote:drsclafani wrote:
phlebologist:
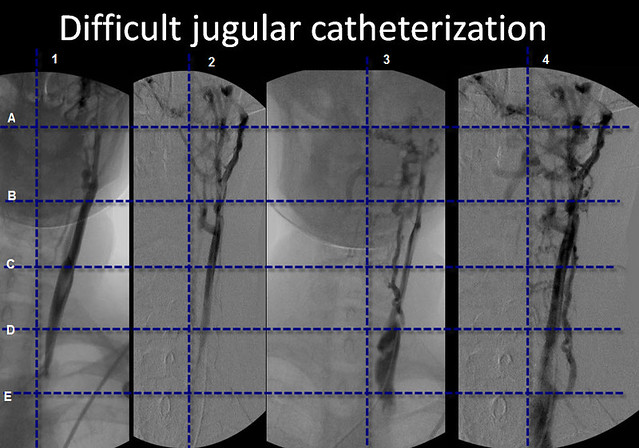
i agree that diameter of right and left ijv are common assymetrical. However, exactly which of these veins do you think is the LIJV. For more clarity among us, i would like some judgement about this. I have taken one of the images and put some grids on it. Would you all point to the closest intersections that show the LIJV
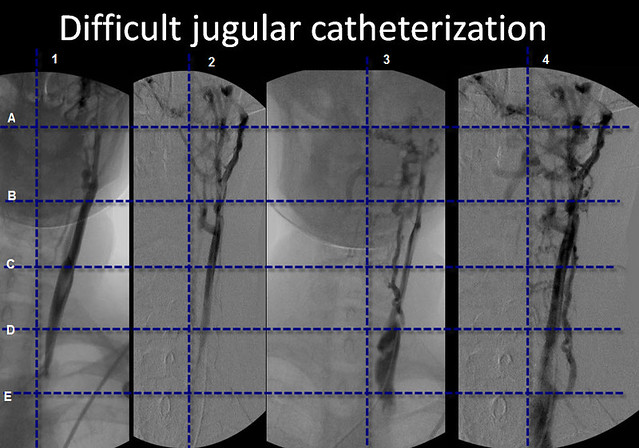
picture 1, square DE1 - catheter is inside left IJV, it cannot be anterior jugular vein, vertebral vein or a cervical vein - look at typical localization of ostium of this vein at the level of medial end of clavicle, also the vein in squares AB1 BC1 and CD1 looks like typical (typical for CCSVI patient), still narrow IJV. However, cranial portion of this vein at pictures 2-4 may be puzzling. The question is: is there a junction with intracranial sinuses.
I guess that there is but the scans are not clear. In a case of doubt - finding a proper way with catheter may be risky (puncture of the vein, etc.). And this is why MRV should be done before the procedure. In most of the cases MRV shows a narrow but existing IJV joining transverse sinus (I've seen only one case of true agenesia at the level of skull base; yet many hypoplasias). Fortunatelly, in most of the cases after dilation of the vein at the level of valve also cranial part of the vein improves (why, being honest - I don't know /it is something more than the flow/). If not - I would suggest local administration of nitroglycerin (sometimes it is vascular spasm caused by catheter).
Re: CASE STUDY #1
Posted: Thu Jan 13, 2011 1:14 pm
by uprightdoc
phlebologist wrote: In most of the cases MRV shows a narrow but existing IJV joining transverse sinus (I've seen only one case of true agenesia at the level of skull base; yet many hypoplasias). Fortunatelly, in most of the cases after dilation of the vein at the level of valve also cranial part of the vein improves (why, being honest - I don't know /it is something more than the flow/).
I have a demo skull in front to me as I write with a mild form of craniosynostosis resulting in hypoplasia of the outlet of the sigmoid sinus which is partially occluded by the petrous portion of the temporal bone. There is also hypoplasia and a split in the hypoglossal canal. On the right side the groove of the sigmoid sinus is deep. The sutures of the temporal bone are obliterated. Conversely on the left hypoplastic side the sutures are wide open when they should have started to close. The sutures are a reflection of stress within the diploic spaces and veins. Open sutures suggest intracranial hydrodynamic stress. The base of the skull is also deviated to the right and there is assymetry of the foramen magnum and condyles.
Dilation of the lower aspect of the IJV creates a void which siphons blood out of the brain the same as upright posture. Unresolved musculoskeletal problems, however, will most likely cause restenosis to occur sooner rather than later.
Posted: Thu Jan 13, 2011 1:25 pm
by uprightdoc
I forgot to include that Dr. Schelling began his research into the role of venous reflux in the cause of MS after noticing significant discrepancies in the size of the jugular foramen in MS patients.
Posted: Thu Jan 13, 2011 3:30 pm
by drsclafani
uprightdoc wrote:I forgot to include that Dr. Schelling began his research into the role of venous reflux in the cause of MS after noticing significant discrepancies in the size of the jugular foramen in MS patients.
can we stay on this case please
Posted: Thu Jan 13, 2011 8:35 pm
by drsclafani
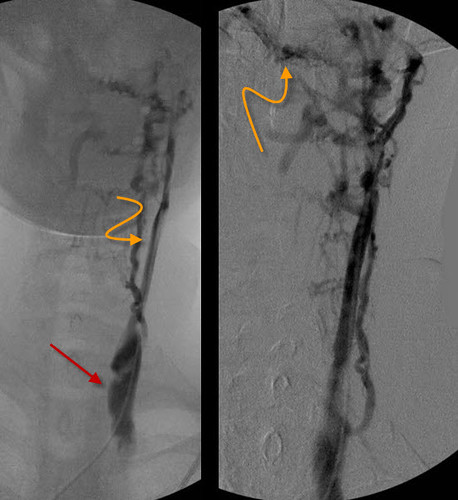
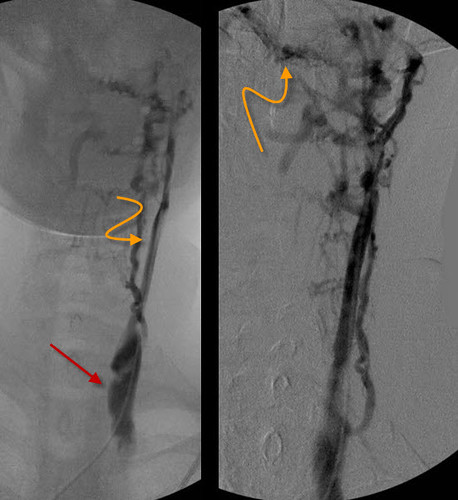
i might be wrong, but i think that the two right sided images identify the jugular vein.
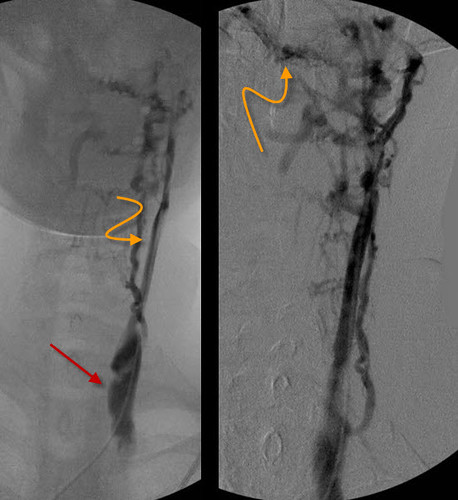
I agree that realtime surface ultrasound could be very helpful in detecting the actual IJV.I chose venography because i am an old fashion angiographer. it is what i grew up with. It was clear to me that the larger structure was the IJV (RED ARROW)
In this case i went for the larger structure. if you follow it cephalad (lower curved orange arrow) i think you can make out the retrograde flow in the sigmoid sinus (upper orange curved arrow).
I don't know what to call that vessel on the left of the original venogram,. I agree, phlebologist, that the vessel on the left images is NOT the anterior jugular vein. i do not know what to name it.
Posted: Fri Jan 14, 2011 12:58 am
by uprightdoc
drsclafani wrote:can we stay on this case please
Regarding this case, we were discussing a possible lack of filling of the left sigmoid sinus and occlusion at the skull base. One possible cause is malformation of the sigmoid sinuses and jugular foramen. Malformations of the base of the skull are common in humans. Another possible reason is mechanical compression due to scoliosis resulting in a head tilt, which has not been ruled out. Additionally, this case has a co-morbidity of RA. RA can cause subluxations of the spine and cervical stenosis. It can also lead to an early death when it affects the upper cervical spine. In this particular case misalignment of the spine may be the cause of poor drainage and ischemia.
Posted: Fri Jan 14, 2011 3:17 am
by phlebologist
drsclafani wrote:.
i do not know what to name it.
I wonder if the vein actually has its anatomical name, I don't think it is the facial vein, it might be one of deep cervical veins, but also it might be an originally very small vessel transformed within years of pathologic outflow conditions into a larger conduit (look at its tortuosity), for sure it is a compensatory outflow route from the IJV and maybe also (is it joining intracranial veins?) from the brain - otherwise it will not fill with contrast.
In Italy or France it will be called a vicarious shunt (I'm not sure if American doctors are familiar with this term)
Posted: Fri Jan 14, 2011 3:43 am
by phlebologist
uprightdoc wrote:drsclafani wrote:uprightdoc wrote:can we stay on this case please
Regarding this case, we were discussing a possible lack of filling of the left sigmoid sinus and occlusion at the skull base. One possible cause is malformation of the sigmoid sinuses and jugular foramen. Malformations of the base of the skull are common in humans. Another possible reason is mechanical compression due to scoliosis resulting in a head tilt, which has not been ruled out. Additionally, this case has a co-morbidity of RA. RA can cause subluxations of the spine and cervical stenosis. It can also lead to an early death when it affects the upper cervical spine. In this particular case misalignment of the spine may be the cause of poor drainage and ischemia.
I disagree. Basing on these pictures you can say nothing about intracranial sinuses - I am sure that the contast has been injected under low pressure (am I right) and consequently contrast will be washed out if the outflow were good, so poor visibility of intracranial sinuses either means that they are not patent, or that they are perfectly OK. On the contrary, in this particular imaging modality well visible transverse sinus means that this vessel is a collateral outflow route from the compromised side.
Moreover, poor visibility of internal jugular vein at the level of skull base most likely does not represent compression by osseous or fibrotic pathology. Rather, it is a result of collapse of the vein secondary to negative transmural pressure. Transmural pressure is the difference between pressure inside the vessel (due to the blood flow forces) and pressure outside (executed by the tissue surrounding blood vessel). Value of transmural pressure is of great importance in a case of the vein, since most of the veins can collapse (thin wall; the exception are veins like inflamed varicose veins, but this is the other story). Since outside pressure remain constant, the vein can collapse when the pressure inside goes down below the value of external pressure. This can be due to gravitational effects (jugular vein in an upright person, saphenous vein with leg elevated, or cubital veins with hand elevated), but also in a case of low flow through the vein (simplified, since in a case of CCSVI perhaps more complex fluid mechanics principles play a role)