Page 4 of 7
Posted: Tue Jan 18, 2011 12:31 am
by uprightdoc
DrCumming wrote:Sal, I think the left IJ maybe occluded at the skull base. I do not see the sigmoid sinus filling.
On that note, I saw a patient treated in Mexico. Imaging was on an ancient 512k cardiac room (no DSA). They ballooned the proximal IJ without looking at the distal IJ. She did not improve. When I imaged here, we found a complete occlusion of the distal IJ at the skull base. Crossed and ballooned that. Modest symptom improvement.
Yes. I am speaking about the case you posted. I used another case to make a point similar to the case Dr. Cummings commented about.
As for stents versus angioplasty, I wasn't advocating either. I was merely pointing out the permanency of certain curvature problems that will most likely cause restenois to occur sooner rather than later due to chronic extravascular musculoskeletal stress. It seems logical that more durable stents would maintain patency longer.
Re: DrSclafani dialogues and debates with other Doctors
Posted: Tue Jan 18, 2011 1:15 am
by uprightdoc
drsclafani wrote:We know there are lurking physicians out there who are curious, learning, trying to get a handle on this liberation thing. Perhaps you are an interventionalist. Perhaps a surgeon, perhaps a physician patient, perhaps a neurologist or family practioner. You know who you are. I know who some of you are. its time to come in, take off your coat and join a physician discussion...I cant promise that the patients won't join in but i ask them to lurk for a change. Perhaps they will learn by hearing our points of views... It's time for more points of view...So I would like to hear from some of you. Lets show the patients that we care and that we struggle on the edge for them.
I certainly care and I have struggled on the edge for decades for patients with neurodegenerative diseases, such as MS, without a red cent in compensation. I offer physicians, scientists and patients a completely different point of view somewhat similar to the theory of CCSVI based on decades of research. I am more than willing to participate and offer my point of view with those who will listen. It is clear, however, you don't really want to hear other points of view so it is pointless for me to be here.
Posted: Tue Jan 18, 2011 4:30 am
by uprightdoc
drsclafani wrote:uprightdoc wrote:stents are not more durable in veins. stents in these veins should be avoided. the track record is not great by most operators. thrombosis is not uncommon, placing stents high near the skull base is associated with cranial nerve injuries as well.
The superior sagittal sinus stays open despite negative intraluminal pressure during upright posture because it is made of dura mater (tough material). I am not claiming to be a vascular specialist but I do know that plastic and metal materials have greater tensile and compression strengh than weak walled veins. I do understand that stents have problems with restenosis due to thrombosis. Likewise angioplasty has problems with restenosis due to collapse. I am not advocating placing stents near the cranial base. Instead, I suggested correction of craniocervical syndromes to relieve chronic venous back pressure (CCVBP).
Posted: Tue Jan 18, 2011 6:57 am
by drsclafani
uprightdoc wrote:DrCumming wrote:Sal, I think the left IJ maybe occluded at the skull base. I do not see the sigmoid sinus filling.
On that note, I saw a patient treated in Mexico. Imaging was on an ancient 512k cardiac room (no DSA). They ballooned the proximal IJ without looking at the distal IJ. She did not improve. When I imaged here, we found a complete occlusion of the distal IJ at the skull base. Crossed and ballooned that. Modest symptom improvement.
Yes. I am speaking about the case you posted. I used another case to make a point similar to the case Dr. Cummings commented about.
As for stents versus angioplasty, I wasn't advocating either. I was merely pointing out the permanency of certain curvature problems that will most likely cause restenois to occur sooner rather than later due to chronic extravascular musculoskeletal stress. It seems logical that more durable stents would maintain patency longer.
do you have any data on the incidence of ms in patients with scoliosis and other spinal malalignments? There were serious consequences of stents placed high near the skull base
stents have added risks of thrombosis
certain stents can collapse
Logic can be a fitful place here
Posted: Tue Jan 18, 2011 7:04 am
by drsclafani
uprightdoc wrote:drsclafani wrote:uprightdoc wrote:stents are not more durable in veins. stents in these veins should be avoided. the track record is not great by most operators. thrombosis is not uncommon, placing stents high near the skull base is associated with cranial nerve injuries as well.
The superior sagittal sinus stays open despite negative intraluminal pressure during upright posture because it is made of dura mater (tough material). I am not claiming to be a vascular specialist but I do know that plastic and metal materials have greater tensile and compression strengh than weak walled veins. I do understand that stents have problems with restenosis due to thrombosis. Likewise angioplasty has problems with restenosis due to collapse. I am not advocating placing stents near the cranial base. Instead, I suggested correction of craniocervical syndromes to relieve chronic venous back pressure (CCVBP).
i got that a couple of pages ago. I havent tried to refute your hypothesis.
The problem is that this patient doesnt even have a known diagnosis of scoliosis or other spinal derangement so i am unclear why you keep coming back to this. I am trying to find out whether the veins in this patient's neck have any anatomical malformation from the images i posted.
i fear that this discussion has morphed into something that none of the physicians care to discuss, much to my dismay.
When i return from ISET, i will complete the imaging of this case to see if i can get some feedback on the imaging and the IR. If other physicians do not care to comment, i will consider this a failed experiment.
Posted: Tue Jan 18, 2011 7:42 am
by DrCumming
Sal, it would probably worthwhile to keep the discussion more focused on the procedural aspects of CCSVI. Not too minimize the discussion of mechanical and alignment issues - its just not within what I think the intent or scope of what you intended this thread for.
Re: CASE STUDY #1
Posted: Tue Jan 18, 2011 8:42 am
by Nunzio
drsclafani wrote:So let's see who come out of the closet!
rule 1: we stay on this case until there are no responses for 24 hours
rule 2. one case discussion at a time
rule 3. patients lurk, comments only by doctors
here goes
The patient is a 33 year old female with short term memory deficiencies, cognitive dysfunction, fatigue, headaches, and imbalance. She has numbness in both hands and the soles of both feet and temperature intolerance. Weakness is predominantly in the lower extremities. She has moderate spasticity, which is worse in the morning. She has co-morbidities of rheumatoid arthritis and multiple sclerosis.
Doppler and B-mode ultrasound of the neck in supine and erect positions and transcranial doppler of the deep cerebral veins was positive for more than one criteria and consistent with CCSVI.
Venography was performed via a left femoral approach.

what is your interpretation?
What would be your next step?
Hi Sal,
first of all I want to congratulate you for establishing this thread.
It is the equivalent of "Grand Rounds" and I hope more IR will present interesting and challenging cases.
I am glad you are routinely entering from the left side. Are you checking the renal vein too?
The picture above from a lumbar vein looks strikingly dissimilar than a normal lumbar vein taken from a presentation of Roberto Galeotti below.
He also reported that in MS patient, specially PPMS, the lumbar plexus looks hypoplastic. Can this be the reason for the poor filling in your picture?
Thanks a lot.

Posted: Tue Jan 18, 2011 9:14 am
by uprightdoc
drsclafani wrote:do you have any data on the incidence of ms in patients with scoliosis and other spinal malalignments?
I have done a cursory retrospective analysis of 25 MS patients who contacted me through this website. Approximately 1/3 of them have significant curvature problems. Another third have history of serious trauma that resulted in measurable misalignments.
CurIous posted his pictures for all to see. He clearly has kyphoscoliosis. Fernando posted his full spine x-ray. He has scoliosis. His symptoms were helped by a heel lift prescribed by his GP. Costumenational posted his upper cervical x-rays which shows severe misalignment of the upper cervical spine. He was in a serious motorcycle accident where he landed on the the side of his head. As I recall all three had ON. I have noticed a fairly consistent pattern of unilateral ON on the low side of the head tilt.
Studies have shown that scoliosis causes functional stenosis and venous congestion and hypertension in the VVP. The veins get compressed against the inside curve of the spine. A study from Rutgers U. further suggested that venous hypertension in the VVP was the most overlooked cause of ischemia of the cord. VVP hypertension in the cervical spine may similarly cause ischemia of the brain. Studies have linked Chiari malformations to trauma and MS, and Chiari malformations have been linked to scoliosis and tethered cord syndromes. Chiari malformations block venous and CSF flow. Functional Chiari malformations due abnormal base and axial-clival angles can likewise compress circulatory problems. Humans are predisposed to Chiari malformations and scoliosis due to upright posture.
It would be cost effective and easy to add plain view x-rays to Dr. Haake's suggested protocols and baseline studies. It could help in understanding the cause of ccsvi as well as the best method of intervention.
Posted: Tue Jan 18, 2011 11:45 am
by phlebologist
uprightdoc wrote:Interestingly, a patient just contacted me regarding assymetry of the superior sagittal sinus connections to the transverse sinuses. The right side is more direct and larger. It also has 5x the flow. Repeat procedures performed in Poland to open the LIJV have failed to significantly improve flow in his case. In cases such as this one, it might be better to increase the siphoning action and flow through the right IJV than to try to improve flow through the weaker left side.
In many CCSVI patients outflow from the brain is very assymetric (easy to demonstrate on MRV). In many cases a textbook confluens sinuum does not exist, on the contrary - superior sagital sinus that carries most of the blood coming from the brain joins only one of the transverse sinuses. We had even a patient with severly blocked internal jugular vein at the level of valve, but this vein actually was draining only the eye, while 99% of blood went to the other side. One can imagine that even after succesfull angioplasty the flow was not much better (I think that putting a stent in such a case is not a good idea).
Posted: Tue Jan 18, 2011 11:53 am
by phlebologist
uprightdoc wrote:drsclafani wrote:do you have any data on the incidence of ms in patients with scoliosis and other spinal malalignments?
I have done a cursory retrospective analysis of 25 MS patients who contacted me through this website. Approximately 1/3 of them have significant curvature problems. Another third have history of serious trauma that resulted in measurable misalignments.
Pathology of skeleton may play a role in CCSVI, but have no evidence that is is a primary problem. Rather, such abnormalities could be secondary to spasticity or another neurologic dysfunction, still, they may play a role in the progression of vascular abnormality.
Posted: Tue Jan 18, 2011 12:02 pm
by phlebologist
uprightdoc wrote:DrCumming wrote:Sal, I think the left IJ maybe occluded at the skull base. ..........................
As for stents versus angioplasty, I wasn't advocating either. I was merely pointing out the permanency of certain curvature problems that will most likely cause restenois to occur sooner rather than later due to chronic extravascular musculoskeletal stress. It seems logical that more durable stents would maintain patency longer.
We have very bad experience with the stents implanted in the upper (cranial) part of IJV. Such a procedure was nearly always associated with a problem (usually, an occlusion, but also: accessory nerve injury, or dislocation of the stent) if not immediately - a problem occured after some time. Now we never stent such lesions, we either use cutting balloons or perform balloon angioplasty in 2 (or more) steps. Importantly, poor INFLOW is a common finding in these (i.e. with stenotic upper IJV) patients.
Posted: Tue Jan 18, 2011 12:18 pm
by uprightdoc
Pathology of skeleton may play a role in CCSVI, but have no evidence that is is a primary problem. Rather, such abnormalities could be secondary to spasticity or another neurologic dysfunction, still, they may play a role in the progression of vascular abnormality.
Likewise for the theory of CCSVI. There is no evidence to indicate CCSVI is the primary problem. Instead, it may be secondary to other problems such as musculoskeletal problems, which is why it shows up later in life like other degenerative conditions such as neurodegenerative diseases. I just referred a patient with EDS-POTS to Dr. Haake and the Hubbard Institute for baseline studies for CCSVI. Among other things, she has hypoplasia of the posterior fossa and possibly the foramen magnum as well along with a pannus formation on the odontoid process of C2 impinging the thecal sac. She has other anomolies as well. RA patients likewise typically have musculoskeletal problems. Some get pannus formation on C2. In some cases C2 migrate into the neural canal.
The theory of CCSVI fails to explain gender, racial and geographic differecnes in the incidence of MS. On the other hand, gender and racial difference in the design of the skull and spine make sense. Winter weather related trauma is most likely the reason for the geograhpic difference.
Posted: Wed Jan 19, 2011 11:39 am
by DrCumming
New case.
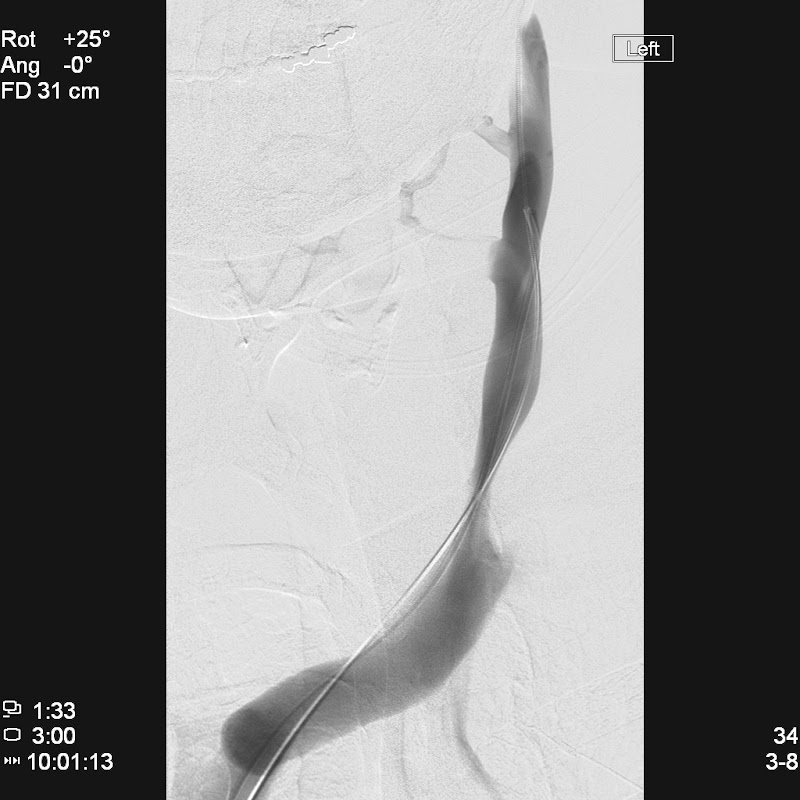
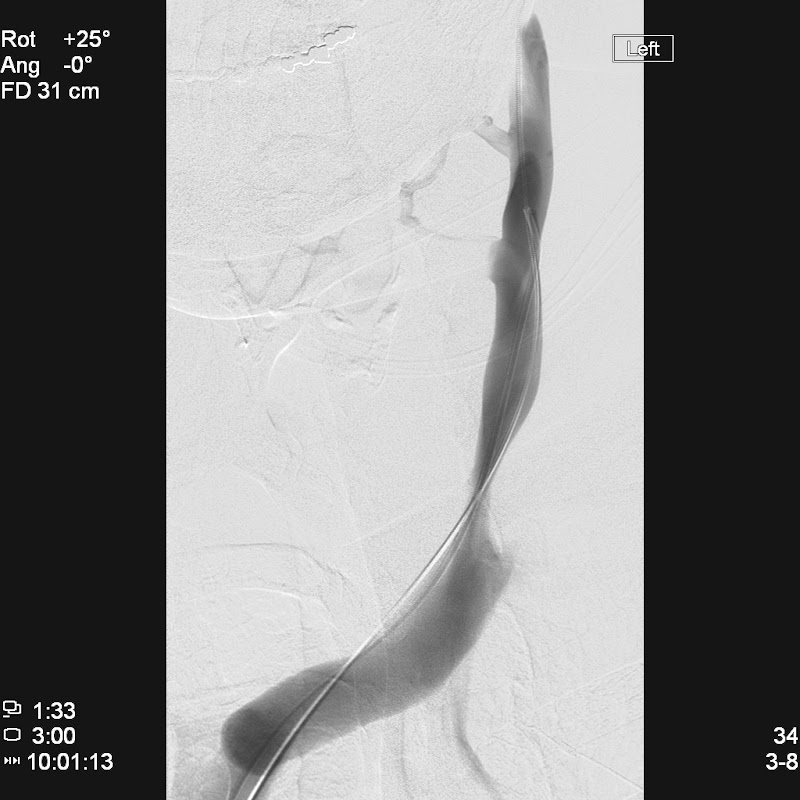
53 yo female with relapsing remitting MS.
Venography showed severe bilateral IJ stenosis and azygous stenosis.
Azygous responded to venoplasty. Both IJ's initially dilated to 14mm. Tight waists in the balloon resolved at 15-18 ATM. Repeat venography showed severe recoil. Multiple repeat dilations, use of a cutting wire and upsizing to 16mm balloon done. Still little improvement in stenosis. Images from left IJ only shown. No clinical improvement at 1 month.
Patient does not want stents (and neither do I).
Thoughts? Options? What would others do differently?
Left IJ preballooning

Cutting wire (after several prolonged conventional balloonings)

Post venoplasty. Severe recoil.
Posted: Fri Jan 21, 2011 9:28 am
by phlebologist
DrCumming wrote:New case.
53 yo female with relapsing remitting MS.
Venography showed severe bilateral IJ stenosis and azygous stenosis.
Azygous responded to venoplasty. Both IJ's initially dilated to 14mm. Tight waists in the balloon resolved at 15-18 ATM. Repeat venography showed severe recoil. Multiple repeat dilations, use of a cutting wire and upsizing to 16mm balloon done. Still little improvement in stenosis. Images from left IJ only shown. No clinical improvement at 1 month.
Patient does not want stents (and neither do I).
Thoughts? Options? What would others do differently?
I don't think that stenting will be a good solution in long-term perspective. Assuming that the stenosis improves only under very high pressure (am I right?) you my expect a very high risk of intimal hyperplasia. If stenting - only stainless steel - not nitinol (higher risk of hyperplasia).
Still, I would suggest to wait a little until big cutting balloons will be available. Companies are working on this topic, we should have the such by the end of this year.
The other problem is that the patients may be a "non-responder" to the treatment for CCSVI.
Posted: Fri Jan 21, 2011 2:59 pm
by drsullivan
How many times did you inflate the balloon, and for how long? I am routinely inflating each stenosis three times, with 2 minute for each inflation.