1eye, you might find Dr. Diana over at her webpage's blog, I notice recent posts from her there:
http://prettyill.com/forums
I wanted to think through some of the ideas Dr. Diana has raised:
* the use of Diamox to reduce cerebral pressure
* people getting CCSVI treatment should be on strict mast cell protocol before/during/after angioplasty
* research can be done on the fundus of the eye to check for CCSVI-induced changes
Here is a link to Dr. Diana's NY symposium talk:
prettyill.com/downloads/CCSVI_Presentation_-_doctors_(2).pptx
Could CCSVI cause a back-up of venous blood that could show up in the ocular fundus, not only given credence to CCSVI, but possibly acting as an inexpensive screening tool for potential CCSVI patients?
An intriguing quote from her description of one of her trials.
Female, age 47, Same eye; note venous irregularity in caliber, stenosis, and see how narrow arteries are. Consider the perfusion coefficient – venous stenosis leading to inability to get oxygenated arterial blood into brain and retina?
I am not yet able to recognise the irregularities she mentions in these slides, but it is fascinating. She listed the pathway from the retina of the eye to the internal jugular vein. It went like this: Capillaries of the retina drain into the central retinal vein drain into the superior ophthalmic vein drain into the cavernous sinus drain into the inferior & superior petrosal sinuses drain into the sigmoid sinus drains into the internal jugular vein.
Here's another concerning quote, from her AAC symposium speech:
42 yr old female – quite disabled. Ignore large vitreous floater and fundus issues related to myopia. Small arteries and veins. 1) is this poor perfusion the reason so many CCSVI patients notice improved vision immediately upon angioplasty? 2) is this a stroke waiting to happen? 3) If this is what perfusion looks like in her fundi, what does perfusion look like in her brain?
I had vision improvement upon angioplasty. Both my eyes improved in their prescription as objectively measured by the machine. I also had improvements in color saturation and distance perception. I am not sure if this was due to improved fundus perfusion?
Hypothesis: “Benign External Hydrocephalus” is not benign at all. Many neurological symptoms in these patients, including delayed motor development, tremors, cataplexy, delayed speech, stuttering, etc.
Do M.S. patients have a “low-level” of high ICP also? If not from birth, when and why did it start? What symptoms can it cause?
Decreased cerebral blood flow secondary to the resulting cerebrovascular resistance when venous or CSF outflow is inhibited. Cerebral blood flow is equal to the cerebral perfusion pressure divided by the cerebrovascular resistance.
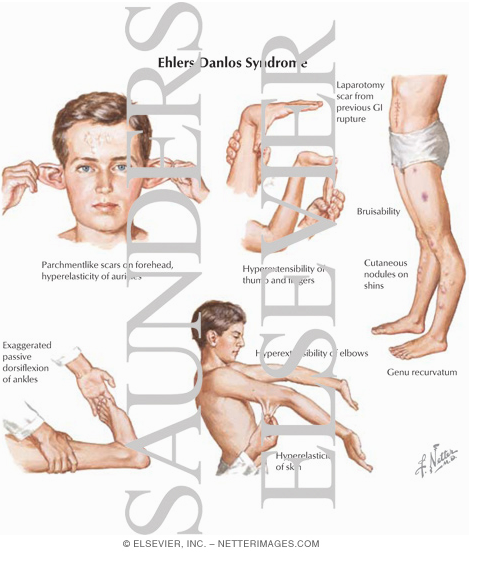
Acetazolamide may have a place in MS tx: is used to treat ischemic strokes, which often causes brain swelling. Even TIA’s can cause brain swelling. How it has been helping patients with dysautonomia and Ehlers-Danlos (and how they often develop MS)
I just checked, and Acetazolamide is Diamox.
“Elevated mast cell tryptase in cerebrospinal fluid of MS patients.”
PMID: 7818259
“Mast cells, T cells, and inhibition by luteolin: implications for the pathogenesis and treatment of M.S.”
PMID: 17713031
“Human mast cells stimulate activated T cells: implications for M.S.”
PMID: 19076366
Some publications to look up. Mast cells are related to MS and can lead to leaky vessels.
And now we're back to mast cells. She has a great image of the change in collagen seen in CCSVI.
Choroid plexus mast cells degranulate, stimulating production of CSF. (Now we have increased production with poor drainage, and possible CCSVI with poor venous drainage).
The condition might create excessive CSF, coupled with the already existing poor drainage due to CCSVI, and we are even worse off. Mast cells are in the choroid plexus, and I've managed to forget what a choroid plexus is.
Oh, and the arachnoid villi may be damaged by long-term high pressure. The arachnoid villi help to drain the cerebrospinal fluid (CSF).
Here she says we have tied together many things, including the cause of pars planitis in CCSVI. I have been diagnosed with unilateral pars planitis (right eye only). First symptoms in my early twenties, diagnosis in my early thirties. She mentions a new proposed treatment for pars planitis, I think she means the Diamox.
edited to add: I notice that Dr. Sclafani added the video of Dr. Diana Driscoll's NY symposium presentation to his page today.
http://www.facebook.com/Sal.Sclafani.MD ... l&filter=1