Page 1 of 2
The problem of occluding stents
Posted: Mon Feb 28, 2011 1:11 pm
by ozarkcanoer
Hello... It's been a while since I have posted but I have a very vexing question. Last August 17 I was treated for CCSVI by Dr Ziv Haskal at the University of Maryland medical center in Baltimore. I told him that it was OK with me if he used stents, especially since the imaging that I had had at BNAC definitely indicated that a stent would be required for my right IJV.
The results of my procedure, that took about 3 hours, was that he found stenosis in both of my IJVs plus stenosis in my azygous. He stented both my IJVs but not my azygous.
In January a colleague of Dr Haskal who is a professor of medicine at Washington University in St Louis performed an ultrasound on my stents and discovered occlusions of about 30% in my right IJV and 80% in my left IJV. Dr Haskal has said he will treat me again... and lucky for me Medicare will pay this time !!!
However the question that bothers me is IF Dr Haskal treats the occlusions, what are the chances that they will just come right back again ? I need to ask Dr Haskal this question, but I hope someone on this board who has stents in their IJVs will have some experience with this. My stents are very high. Dr Haskal used my root canals that show up on the image to position the stents... that is how high they are.
Any ideas, experience or thoughts ?
ozarkcanoer
Posted: Mon Feb 28, 2011 1:47 pm
by Rokkit
Hi OC, I hope you've been well. My stents (also very high and one low) were fine at my one year checkup. I take a baby aspirin every day and I took plavix for 6 months following the procedure. Did you take anything other than aspirin? If not, maybe plavix or something like that would help. If something like that helped you could just take it for life, I think I would. I didn't notice any side effects while I took it.
Posted: Mon Feb 28, 2011 2:17 pm
by DrCumming
Hi OC,
Treating stenosis high in the IJ's is very difficult. Ballooning often does not work as the problems are extrinsic to vein ie. bony and/or muscular structures compress the vein. So, a stent is required to hold the vein open. Likely, you will require repeat interventions to keep the stents open.
Did you get improvement after the procedure? If so, have your symptoms returned?
Posted: Mon Feb 28, 2011 3:32 pm
by Cece
Those are high stents. Hopefully you will hear from some of the original Dake group, they have the most experience.
Will he be treating it by ballooning only or by placing a stent within the stents? I assume it'll be the later, if it's intimal hyperplasia regrowth, since intimal hyperplasia can be thick and resistant to ballooning from what I understand.
Stents irritate the lining of the vein, there's not much that can be done about that, except to get lucky and not be one of the people this happens to. Aspirin, plavix, cod liver oil, fish, exercise might all help.
I am really sorry to hear that you are dealing with this. It's good news about the Medicare.
Dr. Cumming, are you worried when a bone compresses the vein and a stent is put in, that the bone will bend the stent out of shape? We had one patient who had a stent that was bent down like the tip of a funnel, because of the bone it was up against.
I had what looked like a high narrowing, it's why Dr. Sclafani went to the lengths he went to with the IVUS to show that the vein expanded at the end of expiration.
Posted: Mon Feb 28, 2011 3:36 pm
by ozarkcanoer
Hi Rokkit and Dr Cumming !
I took Plavix for 3 months and 1 adult aspirin since. I have taken daily aspirin for about 15 years. I noticed a slight return of my symptoms at about the time I stopped the Plavix but I didn't correlate the two until later. I would be willing to take Plavix for the rest of my life !!! I am now taking Gilenya. The idea of repeated procedures is disheartening

. There is a professor of medicine in St Louis where I live who is performing venoplasty on MS patients, but he won't treat me because I have stents and that is a political "NO" right now. That means repeated trips to Baltimore.
As to how I am feeling.... I had the procedure August 17 but didn't notice a lot of improvement until the beginning of September. I have had the longest running remission of symptoms since I was diagnosed !!! However when I stopped the Plavix, around Thanksgiving, I started to feel a return of fatigue, headaches and burning mouth. But none of my symptoms has ever been as bad as they were last summer before the procedure. I still have my double vision... no change there but with prism lenses that is no problem.
ozarkcanoer
Posted: Mon Feb 28, 2011 3:45 pm
by ozarkcanoer
Hi Cece !!! Dr Haskal is one of the hardest people to contact

I have no idea what he intends to do. He needs several clones. But I am determined to talk to him before I make an appointment and go all the way to Baltimore.
BTW, I had imaging performed at BNAC, both ultrasound and MRV. Both tests showed the right IJV stenosis but not the left. When Dr Haskal was doing the procedure he stented my right side and when he looked at my left side he said it looked just like the right !!!! And he did use IVUS. Another case where US and MRV just didn't work !!
ozarkcanoer
Posted: Mon Feb 28, 2011 4:47 pm
by cheerleader
Hi OC--
I'm sorry you need another go 'round.
Jeff's a high upper, like you. He had serious dural sinus stenosis, too. His right side stent has remained open and flowing at 100%, but his left has been problematic, at one point, deferring to collaterals again. He's needed two repeat angios to reopen the area, and it has been reopened each time. The time between angios has increased. He will be on plavix for life.
The problem is that the area needs good flow and shear stress to endothelialize correctly, and if the flow is sluggish or weak, intimal hyperplasia can form.
Jeff's hydrating, doing cardiovascular exercise 5 times a week, and eating a heart healthy, low calorie diet, including proteolytic enzymes and other supplements in the Endothelial Health program. We hope that the left side will endothelialize as well as the right has. So far, so good for this round. This is a lifetime commitment, just as if you were a heart patient working with a cardiologist...I know, that's hard to hear, but for Jeff--he feels so much better, it's been worth it. I hope it will be for you, too--
cheer
Posted: Tue Mar 01, 2011 6:54 am
by ozarkcanoer
I talked to Dr Haskal this morning and got some good information. Most important is that the sooner these kinds of occlusions are treated the better the outcome. If I wait then scar tissue may form and then it will be untreatable. So I am in the process of making an appointment for Baltimore for a second procedure with Dr Haskal as soon as possible. I'll let you all know how this one turns out !!
ozarkcanoer
Posted: Tue Mar 01, 2011 8:39 am
by Cece
When Dr Haskal was doing the procedure he stented my right side and when he looked at my left side he said it looked just like the right !!!! And he did use IVUS. Another case where US and MRV just didn't work !!
Isn't that interesting, even though it makes imaging studies less accurate! At least the blockages are being found on the gold standard catheter venogram.
All the best with procedure #2. When he says these kinds of occlusions, do you know just what kind of occlusion he means? Occlusions in stents or occlusions from intimal hyperplasia? I've heard mention of scar tissue before, Dr. Arata told a patient that her stent occlusions were all completely scarred and nothing could be done. I know a clot can harden and be like that but can intimal hyperplasia harden? Whatever the details, it drives home the importance of follow-up care and even of ivus, as Dr. Haskal used, to make sure that the area needs treatment.
Posted: Tue Mar 01, 2011 9:11 am
by DrCumming
Cece wrote:
Dr. Cumming, are you worried when a bone compresses the vein and a stent is put in, that the bone will bend the stent out of shape? We had one patient who had a stent that was bent down like the tip of a funnel, because of the bone it was up against.
Bone and time will when that battle.
These narrowings at at the arch of the C1 vertebra are very tough to deal with. In this area it going to be hard to get a good long term result with any approach.
Posted: Tue Mar 01, 2011 10:05 am
by Cece
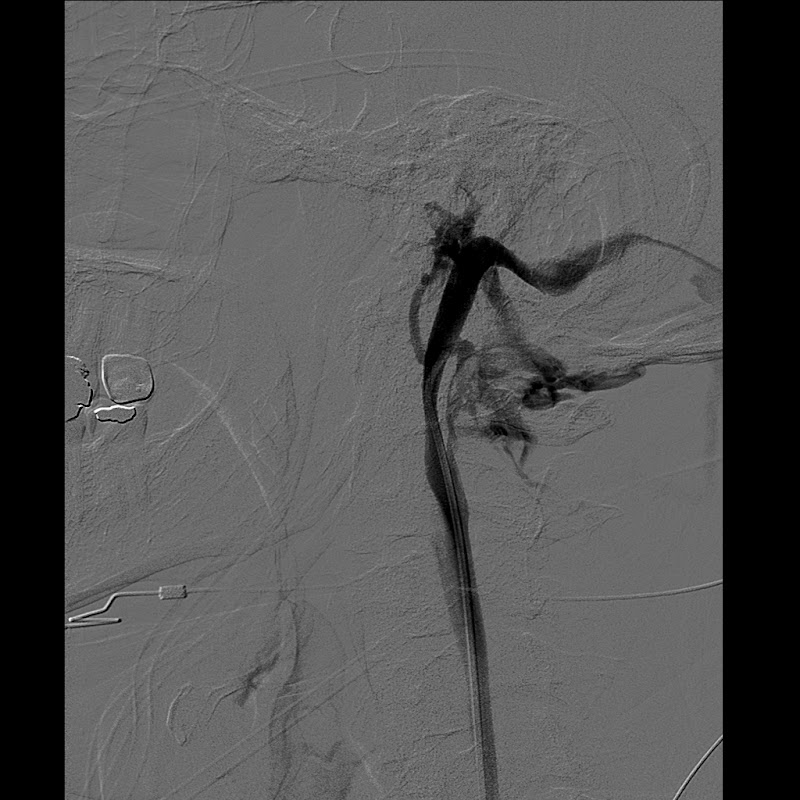
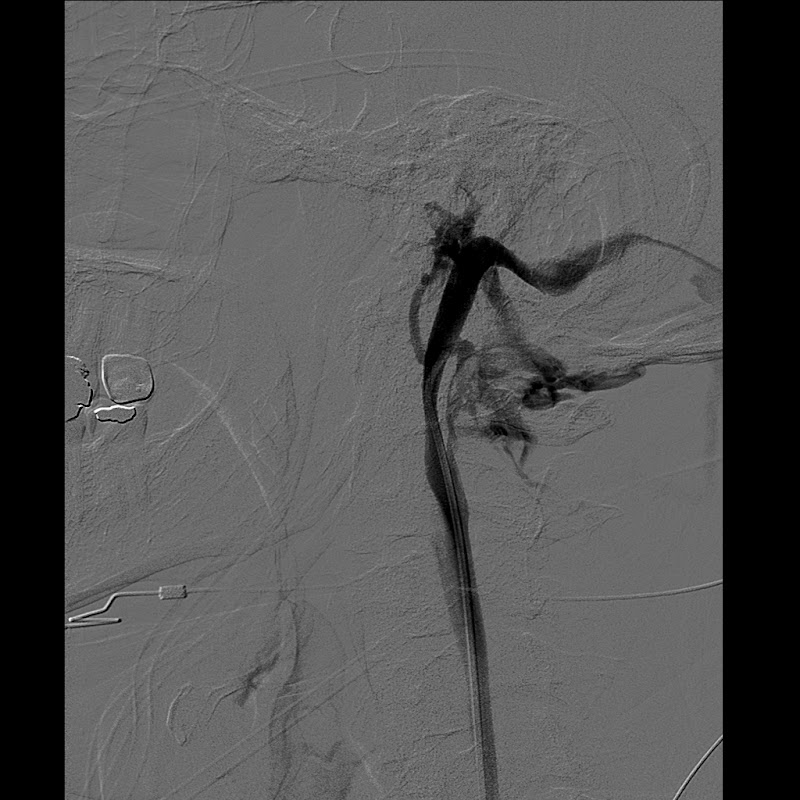
Here's one that a TIMS poster named beechwood posted last year:
http://www.thisisms.com/ftopicp-71898.html
I don't think that can be treated. The other side, with the supposedly missing jugular, it might well be there but not imaged.
Posted: Tue Mar 01, 2011 11:27 am
by ozarkcanoer
Cece... I don't know what kind of occlusion is in my stents. I asked my St Louis IR/professor of medicine at Washington U and he said he cannot tell from the ultrasound what the occlusion is, just that there is an occlusion and about how much

the occlusion is. When I was sitting up and he had the US wand on my left side I could clearly see the diameter of the stent, the occlusion, and the turbulence and reflux of my blood. The other problem my St Louis IR discovered on the US was that my left IJV did not reduce in diameter when I was sitting up. He said "not good". Now I am a bit worried that this won't be fixable. Dr Haskal gave me 3 scenarios this morning. I won't repeat them here but suffice it to say that the sooner I get another procedure the better.
ozarkcanoer
Posted: Tue Mar 01, 2011 11:59 am
by Cece
thanks, ozarkcanoer, it's helpful to understand. Did Dr. Haskal want you to go on blood thinners in the meantime?
I think the blood vessel not changing when you sit up just means that it meets that criteria of the Zamboni criteria, which indicates CCSVI, which is being caused by the blockages in the stents.

I will stop asking questions now though and wish you a quick and successful second procedure.
Posted: Tue Mar 01, 2011 12:20 pm
by 1eye
I would ask, does that mean no blood is flowing through the "upright" veins (spinal) and is there a specific area of my brain that has less flow on that account? I think the answer is no:if you have narrowings in your jugulars, probably all outflow routes have plenty of demand, and so you have more of a problem when you're lying down and should be using jugular routes. Symptoms you acquire overnight.
Posted: Tue Mar 01, 2011 2:53 pm
by prairiegirl
ozarkcanoer wrote: suffice it to say that the sooner I get another procedure the better.
Sorry to hear of your complications, OC. Wish you the very best with your treatment results!