Page 7 of 7
Re: IVUS
Posted: Wed Oct 19, 2011 5:46 pm
by Cece
DrCumming wrote:US at 1 month showed moderate proximal stenosis at the venoplasty site with a residual lumen of 6 mm. Valves were not visible. Preprocedure US showed proximal IJ diameter of 9-10mm.
Was this from scarring? I know "proximal toward the heart, distal toward the brain" but not sure exactly where on the vein, in relation to where the valve was, is meant by proximal. Is it right below the valve or maybe right above it?
Re: IVUS
Posted: Wed Oct 19, 2011 9:28 pm
by drsclafani
DrCumming wrote:1eye, we always check with IVUS and venography after the procedure.
Sal, in this case, do you avoid ballooning the "normal" segment of vein just above the valve? Even with careful balloon positioning how do you avoid having the shoulders of the balloon impacting the normal vein? I am not sure we need to open the valves more than the size of the inflow from the IJ above. My experience has been that most restenosis is from scarring not recurrent valves.
I treated with a 14mm balloon, inflation to 7 ATM. Resolution of the waists in the balloon at 7 ATM. IVUS and venography looked great. US at 1 month showed moderate proximal stenosis at the venoplasty site with a residual lumen of 6 mm. Valves were not visible. Preprocedure US showed proximal IJ diameter of 9-10mm.
I think that the vein can easily tolerate a 50% increase in cross sectional area without injury. My experience in the few patients having second treatments is that the valve restenosis, the vein seems to remain unaffected.
I would have used an 18 mm atlas and pressure up to 16 atm depending upon when the waist opened up.
I would have put the upper shoulder of the balloon as close as possible to the waist and inflated in short intervals no more than 30 seconds.
can you show a post procedure venogram and ivus?
Re: IVUS
Posted: Thu Oct 27, 2011 11:03 am
by DrCumming
Cece wrote:DrCumming wrote:US at 1 month showed moderate proximal stenosis at the venoplasty site with a residual lumen of 6 mm. Valves were not visible. Preprocedure US showed proximal IJ diameter of 9-10mm.
Was this from scarring? I know "proximal toward the heart, distal toward the brain" but not sure exactly where on the vein, in relation to where the valve was, is meant by proximal. Is it right below the valve or maybe right above it?
There is no question, ballooning can cause luminal loss. This is not intimal hyperplasia.
I am not sure exactly sure what the right term is - scarring is probably the best.
It would be great to do a study to determine at which pressure (ATM) and balloon over size that we cause enough injury to the vein wall, that their will be subsequent scarring. My guestimate is that this number is very low even around 5 ATM (assuming of course, that the balloon is larger than the vein).
Re: IVUS
Posted: Thu Oct 27, 2011 3:00 pm
by Cece
Could it be vascular remodeling?
http://www.springerlink.com/content/d24362l822x51571/
It was known in general that the central key of coronary restenosis formation after percutaneous transluminal coronary angioplasty (PTCA) is the intimal hyperplasia resulting from proliferation, migration of smooth muscle cells (SMC), and secretion and synthesis of extracellular matrix (ECM). But the indefinite effect of all kinds of measure for inhibiting intimal hyperplasia in reducing occurrence of restenosis urged people to reconsider the pathogenesis of restenosis. Since 1993, some studies in using quantitative histological or intravascular ultrasound methods have shown that apart from intimal hyperplasia, vascular remodeling also plays a part in the pathogenesis of restenosis and might be the major mechanism of it.
Re: IVUS
Posted: Sat Oct 29, 2011 4:20 pm
by DrCumming
Cece wrote:Could it be vascular remodeling?
http://www.springerlink.com/content/d24362l822x51571/
It was known in general that the central key of coronary restenosis formation after percutaneous transluminal coronary angioplasty (PTCA) is the intimal hyperplasia resulting from proliferation, migration of smooth muscle cells (SMC), and secretion and synthesis of extracellular matrix (ECM). But the indefinite effect of all kinds of measure for inhibiting intimal hyperplasia in reducing occurrence of restenosis urged people to reconsider the pathogenesis of restenosis. Since 1993, some studies in using quantitative histological or intravascular ultrasound methods have shown that apart from intimal hyperplasia, vascular remodeling also plays a part in the pathogenesis of restenosis and might be the major mechanism of it.
In arteries yes, for veins, in this situation, still think scarring is a better term. Sal?
Re: IVUS
Posted: Mon Oct 31, 2011 2:45 pm
by drsclafani
DrCumming wrote:Cece wrote:Could it be vascular remodeling?
http://www.springerlink.com/content/d24362l822x51571/
It was known in general that the central key of coronary restenosis formation after percutaneous transluminal coronary angioplasty (PTCA) is the intimal hyperplasia resulting from proliferation, migration of smooth muscle cells (SMC), and secretion and synthesis of extracellular matrix (ECM). But the indefinite effect of all kinds of measure for inhibiting intimal hyperplasia in reducing occurrence of restenosis urged people to reconsider the pathogenesis of restenosis. Since 1993, some studies in using quantitative histological or intravascular ultrasound methods have shown that apart from intimal hyperplasia, vascular remodeling also plays a part in the pathogenesis of restenosis and might be the major mechanism of it.
In arteries yes, for veins, in this situation, still think scarring is a better term. Sal?
mike, i am just not seeing what you are speaking about. About 25% of my patients are retreatments done by somebody else between june 2010 and july 2011. the only restenoses I have noted have been at the site of angioplasty and it appears to be at the valves
Case 8
Posted: Wed Nov 02, 2011 5:39 am
by DrCumming
Hi Sal,
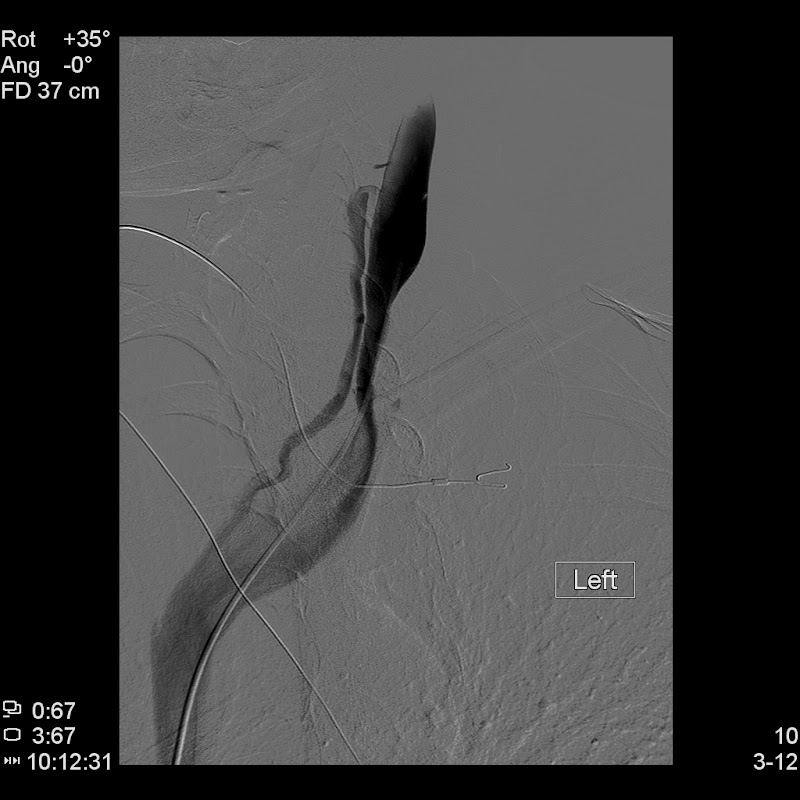
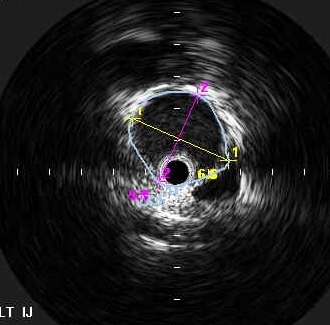
Here is a case to illustrate what I have seen. I did this procedure shortly after the EHC meeting in Glasgow. At that meeting there was a lot of enthusiasm for big balloons and having to break the annulus using cutting wires if needed. I was not using IVUS at this time.

Used a 14 mm balloon. Needed a cutting wire to get the balloon to inflate to profile.
Patient had significant improvement in symptoms. US of left IJ below is at 1 month. Right side (not shown) looked great. Patient still doing well. US shows severe luminal loss in the left IJ at the venoplasty site. There is thickening in the vein wall (?edema). No thrombus.

and

Patient continued to do well clinically for 9 more months, with gradual worsening in the last 2 of those months.
Venography and IVUS below of the left IJ
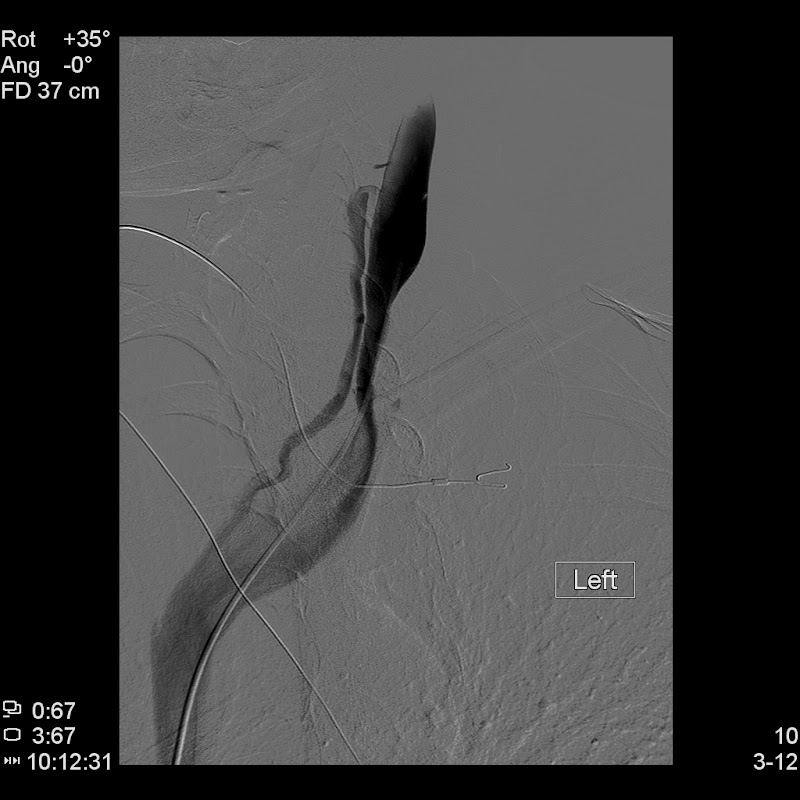
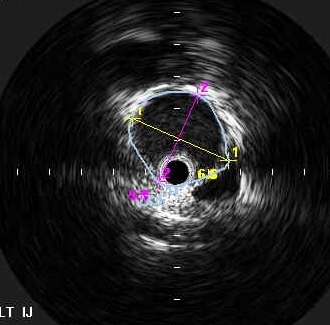
The stenosis/restenosis is due to luminal loss in the size of the vein. Not intimal hyperplasia or recurrent/undertreated valves.
I have seen this mode of failure more commonly than recurrent valves. This has to be from too aggressive of a venoplasty.
Re: IVUS
Posted: Wed Nov 02, 2011 7:36 am
by Cece
In this case, was the stenosed area able to be redone?
If a vein now presented the way this one initially did, I'm assuming you would not be as aggressive, which gets to the question you've been raising about endpoints. It would have required stopping while narrowing remained?
Dr. Sclafani was prognosticating that in the next year or two, we will see more papers on the finer details of techniques (as well as RCTs and other research). It was the finer details that interest me, since I am already satisfied of the association between MS and CCSVI, and that we are better off without blockages than we are with them, and that angioplasty is the treatment of choice for venous blockages. But optimizing the techniques could lead to improvements in efficacy, safety, and durability. With the high pressure balloons, it would be helpful to see veins where everything was done "right" with the only variable being the use of high pressure or not, and follow-up images as well.
Re: IVUS
Posted: Wed Nov 02, 2011 8:09 am
by DrCumming
Yes, we did retreat, smaller balloon, lower pressures and the patient continues to do well.
We really need further investigation in an animal model to determine how much force we can apply to vein wall without damaging the structural integrity of the vein and subsequent loss of luminal diameter due to "scarring".