Page 2 of 3
Response to Plavix Aspirin question
Posted: Mon Jul 11, 2011 6:04 am
by DrSnyder
Dear Z -
Thank you for your kind words.
OK - I need to begin by advising you to speak with Dr. Cumming on this as he is your managing physician, and also to place a warning that I am speaking in generalities and not giving you specific medical advice as a patient. This is necessary so, 1 - I am acting within the moral confines of the patient/physician relationship, and 2 - since I do not have your full medical history or any info about you short of what you have shared here in which to modify any opinions.
The folks who told you the difference between Plavix and Coumadin were correct.
Plavix generally inhibits platelet aggregation. Platelets are the smallest part of the circulating blood stream that bind together in order to form a clot. It is the aggregation of these platelets when they join together and forms a physical "net" that trapped the red blood cells and begin the formation of a clot.Generally when we place stents on the arterial side, we will place a patient on Plavix short term (3 months) to reduce platelet aggregation. Most of the good data we have are from cardiac stents. To a large extent, Plavix (clopidogrel) is like a glorified aspirin. They both work in the same way. There are a few useful studies (again on the heart) that shows it works slightly better than aspirin for keeping the heart arteries open.
So Plavix will make it harder to form a clot by stopping the first step in it's creation.
Coumadin, on the other hand, works on the liver to reduce certain blood clotting proteins that we use to build a clot. Generally, we will use Coumadin long-term (or Lovenox/heparin on the short-term) to prevent clotting on the venous side.
I will generally put my venous stent pateints on coumadin either for three months or longer if there are clotting issues.
I have one patient whom I am very fond of who we have put on dabigatran since the coumadin didn't seem to be working.
So - after the lecture, what are you left with?
1. Yes - Plavix = Aspirin - good for the arterial side
2. Coumadin - good for the venous side.
Sometimes we will do both in the absence of strong clinical data to try to ensure a good outcome. Sound familiar?
I would say in the end, trust your Doctor and ask lots of questions. Lots of questions!
Best regards -
Greg Snyder
Posted: Tue Jul 12, 2011 8:05 am
by zinamaria
Hi Dr Snyder,
Thank you so very much for taking the time to respond to my question, I greatly appreciate it. Please know that I (we here at Tims) are honored to even have doctors come on board to interact with us and to answer questions; that the contributions are so utterly valuable to us as it is not standard practice to have such a doctor/patient exchange of information, where the doctor is truly listening and only not 'telling', and yet we want to be 'told' for the majority of us here are very involved in the disease that plagues our lives, and are trying as best we can to understand its complexity, now in including CCSVI.
On that note!....it seems that bruising is par for the course with these medications? I was told this about plavix, and I see the spontaneous small bruises surfacing on my body.
My next question is this: if I want a professional massage, am I at risk at all with that kind of body manipulation while on this medication? I hope this is not the most ridiculous of questions, but I thought if I am bruising without falling or bumping into anything (thank goodness!) but they are occurring, what about someone digging into my muscles etc...?
Once again, thank you,
Z
Professional Massage
Posted: Tue Jul 12, 2011 10:29 am
by DrSnyder
In my opinion you should be fine with a massage.
Let them know about the medication, but likely it won't matter at all unless they are REALLY aggressive.
I would also avoid massage directly over the jugular veins.
No science here, just seems like a good idea...
Best regards-
Greg Snyder
Procedure images
Posted: Tue Jul 12, 2011 1:34 pm
by DrCumming
Better late then never... sorry for the delay uploading these!
Images from both IJ's
Very classic findings. Bilateral IJ stenosis secondary to poorly opening valve leaflets. Excellent examples of using IVUS for pre and post ballooning.
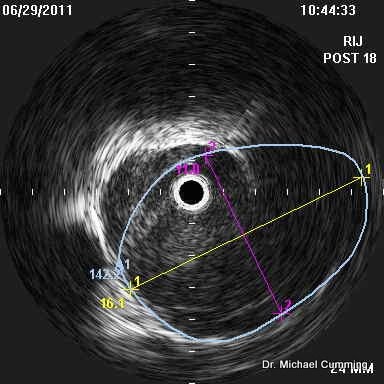
Right:
This side is dominant.
Venogram prior to ballooning showing the stenosis at the level of the expected location of the valve plane.

and IVUS better showing the valves and the size of the normal vein at the level of the valves. Knowing this allows better selection of balloon size.
Area at valves is 96 mm sq

Vein at this level is 160 mm sq

Initial ballooning was 16 mm. This was suboptimal on IVUS. Next ballooning was 18mm. Repeat IVUS shows improvement to 142 mm sq. Up for debate is should I have gone larger. Note in the top right corner, the valve leaflet is still not completely open. I do not have a good answer. The enemy of good is perfect so I elected to leave this alone. Its a substantial improvement from the original area of 96mm sq
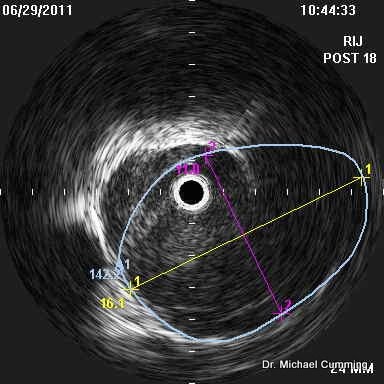
Post 18mm venogram looks good. You can see the one leaflet that is still not 100% open.

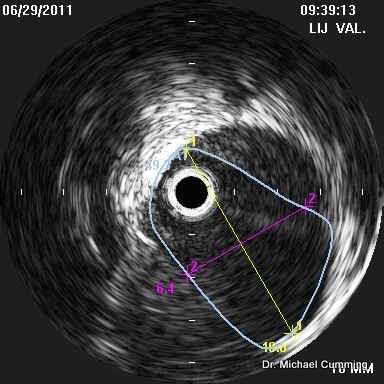
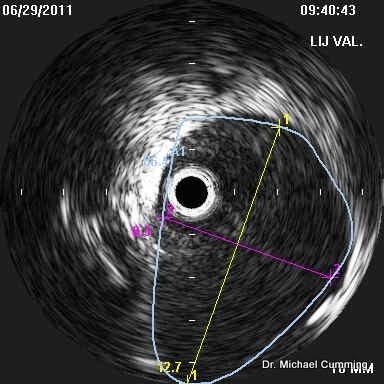
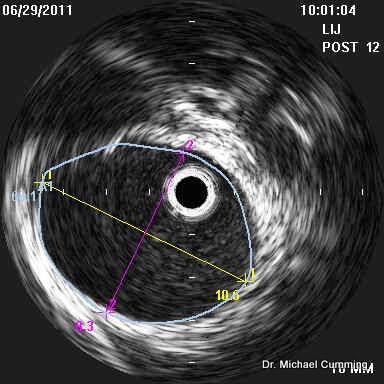
Left:
This side is smaller then the right but not hypoplastic.
Venography shows no real narrowing. Yes, the vein does narrow as it enters the low neck. Trying to make this segment of vein look like the mid portion of the IJ will often result in occlusion or severe restenosis. See discussion below.

But IVUS at the valve plane shows the incompletely opening valve leaflets with an area of 49 mm sq.
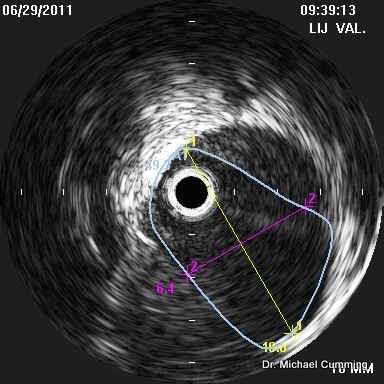
The area of the jugular vein at this level is 96 mm sq.
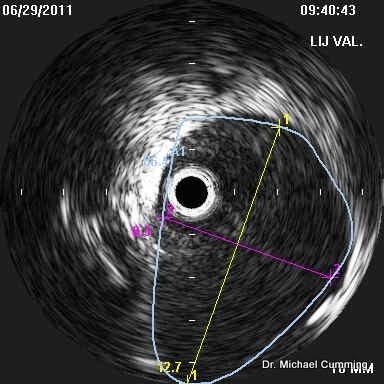
The area of the jugular vein just above the valve plane is 62 mm sq (Not shown).
So, this raises some interested questions about how to treat the left side.
1. Do we make the opening of the valves equal to the area of the jugular vein immediately distal?
2. Make the valves open to the size of the vein at the level of the valves? Can we do this without causing significant injury to the "normal" smaller jugular vein just distal to the valves?
3. Make the entire proximal segment of the jugular vein as big as the mid portion of the jugular vein?
Number 3 in my experience often results in occlusion or severe restenosis. I do not do this anymore.
So, we are left with 1 and 2. 1 is definitely going to be the less traumatic option (in terms of intimal injury). But may not result in optimal treatment benefit. Option 2 may work, but also may cause too much intimal injuryto the vein just distal. I don't have a good answer but I was requested to do the procedure to minimize risk. So I chose option 1.
Initial dilation to 10 mm did not improve the area. Dilation to 12 mm improved the area to 62 mm sq.
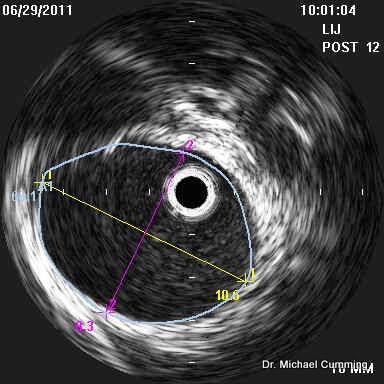
And post venogram is not all that different (as expected).

So, some very good images and examples of the complexity of the decision making behind these procedures and the many things we do not know. Yet.
Being overaggressive.
Posted: Tue Jul 12, 2011 2:00 pm
by DrSnyder
I agree completely with Dr. Cumming on not being overaggressive in these cases. One of the most difficult cases that I am still treating is a case where the jugular vein was likely overdilated causing a dissection which lead to stenting and then the patient was not anticoagulated. This has caused some great havoc in trying to open the stent and maintain patency. In my opinion until we have a better understanding about which patients will truly benefit from the procedure, I am hesitant to do anything to injure the vessel wall.
Nice IVUS pictures Mike! Are you billing that out separately or as a modifier?
In my experience so car we have had very good luck in getting insurance coverage but I do suspect to some degree that it is because they don't fully understand what it is we are doing. I can only imagine as this becomes more prevalent that they will find a reason to deny coverage.
Best regards,
Greg Snyder
Posted: Tue Jul 12, 2011 2:22 pm
by cheerleader
Wow! Incredible images. Dr. Cumming and Dr. Snyder--if you're not already over at the Endovascular Forum, I'd love to invite you to come and post your cases for your colleagues. The doctors are all learning from each other, and IVUS are an important part of the understanding. CCSVI Alliance (the non-profit I work with) has a presence on there.
http://www.endovascular.org/
As the wife who brought Dr. Zamboni's paper to Stanford, where my husband was treated over two years ago, I am astounded at how much we are learning.
thanks for your visits here and the information- and congrats to Zinamaria for her research and determination. Continued healing!
cheer
Posted: Tue Jul 12, 2011 7:42 pm
by Cece
Conversely, I'd love for their colleagues to come and join the conversation here.
I cannot say enough how much at TIMS we benefit from the discussion on this level.
I agree about the insurance. In some states, BCBS has a drafted policy specifically addressing CCSVI in MS as investigational and not covered. Fortunately this has not happened in Minnesota yet. (I am from MN so have a vested interest in all things MN and CCSVI.)
I have heard it mentioned lately, that we do not yet know which patients will benefit and which won't. If there was a pattern, wouldn't it have shown up by now?
Dr. Cumming, I am glad for the 'yet' at the end of your statement of there being so many things we do not know. It is encouraging to know that CCSVI is a work in progress and the answers will be coming. It is still early days. Great images, btw, and some difficult questions raised.
What we don't know...
Posted: Tue Jul 12, 2011 8:38 pm
by DrSnyder
Dear Cece
Great idea about posting my cases. I will contact my patients and get their approval since even though the data would be annonymized the CCSVI community is small enough that everyone seems to know everyone else.
In regards to your question, don't we know who benefits, the answer remains "not yet." Getting objective data in a controlled randomized fashion is going to be difficult because who really wants to sign up for the "sham" procedure if the actual procedure might confer benefit. To get the truly good data we would have to do it that way.
I will say that anecdotally every one that I have treated has reported some benefit usually in ambulation and endurance.
I remain very encouraged.
Best regards
Greg Snyder
Posted: Wed Jul 13, 2011 7:39 am
by zinamaria
Wow! Two for one, I like it! Thank you Dr. Snyder for the feedback on massage; in fact my sister (who is visiting and is a certified massage therapist) was only doing shoulders and went she went to the neck I too told her to stay away...she has VERY strong hands! It also was just an intuition
AND Dr. Cummming so great to have you post these images, amazing! I too, as Cece said, really like that 'yet' at the end of that sentence.
I am thankful for your prudence as regards the procedure; it only 'seems' from the images and what you say that IR's 'could' do more, and 'yet' how do we know, and to what extent do we take risks? Landing on the side of prudence makes sense to me.
Do either on of you think that May Thurner is connected to CCSVI in terms of the complications that you are finding on the left side? How often do you find it while treating CCSVI? Or do you? Any thoughts on it?
After my food poisoning bout I was concerned I was back to square on (it was a horribly draining two days sick in bed) BUT three days have passed and I am feeling great, again the energy levels seem to be the greatest change. Just even having my sister here is a big deal for me, for her levels of energy usually drain me, even just on the phone. We are out doing things and spending a lot of time together and fatigue hardly comes up.
Of course, I am resting the minute I get a hint of that need.
On a side note (always a side note) I found this in my reading yesterday:
"So in my veins red life may stream again"-----Keats
Re: What we don't know...
Posted: Wed Jul 13, 2011 2:05 pm
by Cece
DrSnyder wrote:Dear Cece
Great idea about posting my cases. I will contact my patients and get their approval since even though the data would be annonymized the CCSVI community is small enough that everyone seems to know everyone else.
In regards to your question, don't we know who benefits, the answer remains "not yet." Getting objective data in a controlled randomized fashion is going to be difficult because who really wants to sign up for the "sham" procedure if the actual procedure might confer benefit. To get the truly good data we would have to do it that way.
I will say that anecdotally every one that I have treated has reported some benefit usually in ambulation and endurance.
I remain very encouraged.
Best regards
Greg Snyder
The situation in Canada, where the procedure is not locally available, might be perfect then for clinical trials. Here in the US, where the procedure is available, less perfect. Fortunately Canada is going forward with trials.
I look forward to seeing your cases!
Posted: Thu Jul 14, 2011 8:43 pm
by zinamaria
Dr. Snyder,
I too hope you post cases.
It does seem as if no one would want to participate in a trial that needs to use 'sham' procedures, and makes sense, as life with MS too hard to think something that may benefit might not have happened.
Is there just no alternative?
It is refreshing to hear that your experience with the procedure is that there are benefits for those you treat.
Z
Posted: Tue Aug 02, 2011 8:05 am
by JCB
Dr. Snyder,
I am sure your patients wouldn't mind you posting some pictures. If we can move this science forward (or understand it a little better) everyone gains. Besides if you just looked at my images for instances, you might think I am a good looking guy. So I don't think anonymity will be that big an issue.
We all just want to get better, and even stopping progression is better.
They say that doing the same thing over and over while expecting a different result is lunacy. I am tired of lunacy, let's try something different, even if it sounds crazy to some. In my mind it is crazy not to pursue.
Jim
Posted: Tue Aug 02, 2011 9:59 am
by zinamaria
Glad you bumped this thread Jim for I wanted to post my most recent adventures post angio.
My symptoms are still much the same, numbness in hands, especially the left, still some balance issues. But I do have much much more energy. And if feels as though I am stronger, notwithstanding the smaller issues. Not nearly as much fatigue. I have just decided for myself that MS is an circulation issue, that's just how it seems to me.
This last weekend I went on my first trip out of town...ALONE. First time traveling alone in three yrs. I was a little anxious at first, but that fell to the side as I proceeded to drive myself from Santa Fe to Alb the night before departure where I stayed at a hotel.
Next morning took the shuttle to the airport and managed it all by myself, from getting the boarding pass to getting through security and then to the gate. Was not overwhelmed and the airport was packed. I did give myself a lot of extra time as I still walk slowly. But it was all so smooth navigating and decision making etc.
To do all this without my companion was a huge success.
Was off to San Diego where my 90yr old friend had an opening to his last gallery exhibit. He has been a painter his life entire and I was not about to miss this event, but I can tell you that I was not sure I would go until about two weeks beforehand for I knew I would have to go alone for my companion could not leave due to work. So it felt like a huge risk/test of strength, mental and physical.
I did not drive in San Diego, but not only did we (was with cousins) spend the evening at the show, we were up until midnight, and I slept soundly until we were up again at 8am and off to the Getty Museum. Sunday we were out 12hrs! A first for me and I did so much walking that day although took the needed rests and elevators, but still was out in the world doing it all!
The only weak spot in the entire trip was that I had bowel incontinence on the way home and was so happy to make it to the rest stop just in time. This has been a problem and am not sure if it's the MS/CCSVI or bad dieting or both. Thank goodness my cousin's empathy was right there, her 76 yr old husband has similar issues so they understood.
That's the update.
Z
Posted: Tue Aug 02, 2011 11:10 am
by 1eye
It seems to me that jugular valves are a Good Thing. They don't get used much because we spend most of our time not upside-down. Maybe that's why they get stenotic, or fused, or hypoplastic.
Jugulars are used for spinal fluid shunts for hydrocephalus. Here a valve has to be put in to prevent too much downward flow, which would result in loss of too much spinal fluid.
These devices are worn inside jugulars for a lifetime. It seems to me, especially for people like me whose lifetimes are going to be shorter because of 'MS' anyway, and who are of 'significant' age already, a plastic stent with a man-made valve in it would be fine. If it were big enough I would never have any problem draining overheated blood from my head. Maybe a valve like the hydrocephalus shunt one would prevent fainting from too much drainage.
Posted: Tue Aug 02, 2011 12:16 pm
by Cece
1eye, I'm not sure which doctor it was, but one of the doctors at the AAC symposium was discussing hydrocephalus in MS. Apparently the two are associated. Maybe due to the effects of jugular blockage on CSF flow. Shunting is a solution. I thought of you and your brother's case as soon as it was mentioned, which was in Arlene Hubbard's notes on the event.