It does not surprise me that there has not been models done of the head and neck veins. Such an under-researched area.
I will have to read the linked articles slowly, as I am poorly acquainted with both newtonian and nonnewtonian fluid dynamics, and Reynolds numbers, and vortex shedding.
http://virtual2002.tau.ac.il/users/www/ ... enosis.pdf
X-ray Angiography is error-prone when the vessel is noncircular, because it uses a projection view of the geometry.
Dr. Cumming showed us an azygous that looked stenotic by angiography, but nonstenotic by IVUS, because of the oval (noncircular) shape of the vein.
Experimental studies of stenotic vessels have typically focused
on the flow downstream of the stenosis, particularly on the disturbance
produced by the stenosis and whether the resulting flow is
turbulent, not on the mechanisms of plaque rupture.
In CCSVI, what we are interested in is the effect of the stenosis on the upstream flow. Downstream has been virtually ignored.
Here's an entirely different article, on downstream effects:
http://www.sciencedirect.com/science/ar ... 8404002084
Venous Flow Restriction: The Role of Vein Wall Motion in Venous Admixture
S Raju , , G Cruse, M Berry, S Owen, E.F Meydrech, P.N Neglen
River Oaks Hospital and University of Mississippi Medical Center, Jackson, MS, USA
Accepted 21 April 2004. Available online 7 June 2004.
Abstract
Objectives. There are wide differences in flow between vascular beds at rest, even more during stress. The hydrodynamic energy (Energy grade line or EGL) of venous outflows must also vary considerably between vascular beds. We explored the mechanism of venous admixture of differing energy flows using a mechanical model.
Materials and methods. The model simulated two venous flows coalescing at a venous junction and then flowing through collapsible venous pumps. Flow rates and pressures were monitored when the venous pumps were full (steady state) and when they were compressed and allowed to refill inducing wall motion (pump flow).
Results. With increasing EGL differences between two coalescing venous flows, reduction or cessation (venous flow restriction) of the weaker flow occurred during steady state; higher base EGL of both flows ameliorated venous flow restriction and lower base EGL the opposite. Outflow obstruction favoured venous flow restriction. Pump action in the vicinity of the venous junction abolished venous flow restriction and maximized both venous flows.
Conclusion. The model suggests a pivotal role for vein wall motion in venous admixture and regional perfusion. Observations in the model are explained on the basis of network flow principles and collapsible tube mechanics.
This one discusses outflow obstructions and veins, in a mechanical model. Dr. Raju and Dr. Neglen are experts in May Thurner syndrome. The base of the jugular, where valvular obstructions are, flows into the subclavian so looking at subsequent admixture might be possibly relevant. My limited understanding of this article is that the weaker flow coming from the occluded jugular would be further weakened by competition for flow in the faster-moving subclavian, further reducing outflow from the jugular. The pump would be the thoracic pump. Vein wall motion is greatly affected by elasticity of the vein, and females have less elasticity than males.
Ok, that's a thought on downstream flow.
Back to the first article....
Morphological details of diseased vessels, such as surface irregularity and stenosis curvature, have been shown to have important effects on the blood flow.
If a plaque is like a curved speed bump on the artery wall, wouldn't a fixed valve leaflet be more like a straight-out road block? If curvature matters, I would expect these sorts of stenoses to have a greater effect on flow.
Both pressure and velocity distributions are similar for all three
Reynolds numbers, with magnitudes of both pressure and velocity
increasing with Re. Figure 5 shows the contours of total pressure
~static plus dynamic pressure! for this range of Reynolds numbers.
A large pressure force acts on the wall just upstream of the stenosis
throat in the internal carotid artery.
There's a large pressure effect, just upstream. Interesting.
At diastole, vortex shedding
is observed from the shoulder of the carotid sinus, far upstream of
the most severe occlusion. The vortex that has formed at t50.230
seconds has detached by t50.290 seconds. This shed vortex is
carried into the sinus, where it dissipates. Another vortex has
formed at the shoulder by t50.50 seconds. This would indicate a
shedding frequency of 3.7 Hz, or a Strouhal number of 0.84 to
1.0.
ok, vortex shedding must be flow or pressure effects upstream or downstream of the stenosis itself. I don't want vortex shedding in my dural sinuses or capillaries of the brain.
The assumption of Newtonian
behavior may break down when the shear rate is low
(;0.1 s21!, for example in small arteries and downstream of
stenoses. In some diseased conditions, including atherosclerosis,
blood exhibits some non-Newtonian behavior @38,39#. The effects
of non-Newtonian behavior on flows in stenotic vessels are first
considered for axisymmetric 50 percent stenoses
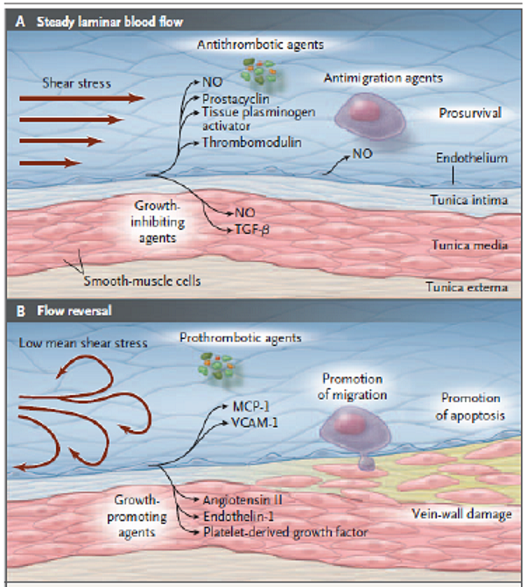
here we get to what's relevant to the shear stress diagram that I posted. What happens when the shear stress drops? We're also reading about arteries, which are high flow, which might not be directly applicable to veins, which are low flow.
The advanced lesion experiences a dramatically different flow
field from that of a healthy artery or one in the early stages of
atherogenesis. Fluid shear stress in undiseased arteries ~comparable
in size to the common carotid artery! is on the order of
1–2 N/m2, while endothelial cells in the throat of a tight stenosis
may experience shear stresses greater than 30 N/m2. As
Fry observed, shear stresses in this range may severely damage
endothelial cells, or even strip them from the vessel wall.
Tensile wall stresses, distributed evenly around the circumference
of a healthy vessel, are likely to be focused at the most vulnerable
shoulder regions of a diseased vessel @43#. ~The ‘‘shoulder regions’’
contain transitions from normal to diseased artery wall.!
This is discussing high shear stress, and the reason why plaques often rupture upstream of the point of maximum stenosis, and not at the maximum stenosis itself.
Gosh this is interesting. If the highest pressure is just upstream of the stenosis, then those of us with lower jugular stenoses may have been better off than those with high jugular stenoses, who may have a more complicated situation with the pressure being highest just upstream of that high jugular stenosis at an area much closer to the dural sinuses and the brain.
A k-v model such as that of
Wilcox, also given high marks by Patel et al., may be more
suitable than k-e models for flows in stenotic vessels.
k-v, not k-e
Our vessels are definitely stenotic.
My understanding of shear stress has only been of the effects of low shear stress, as seen in the diagram I linked. But this article talked about high shear stress existing at the site the stenosis itself, which makes sense, if flow velocity increases past the stenosis. The shear stress can be high enough to tear endothelial cells right off? Perhaps this is only true in high flow arteries, not low flow veins.
I am sure I did not understand nearly as much as I could have of this article, if I had the background, but it seems relevant to apply such mathematical concepts to CCSVI. I would like to see just what effect my bilateral stenoses (77% and 99%) had on the flow and pressure points upstream. An IR once suggested to a TiMSer who had a fully occluded vein that they might be better off with a full occlusion than with a partial occlusion. This seems nonintuitive, and obviously more outflow will be obstructed with a full occlusion than with a partial one, but it is possible that the full occlusion results in less reflux and less focal hypertension than a partial occlusion would. A mathematical model might help answer that question.