Page 1 of 3
Stent fears inhibit good care sometimes
Posted: Fri Feb 24, 2012 11:22 pm
by drsclafani
Today i had a very unfortunate case. I was unable to perform stenting of a renal vein obstruction because the patient had a bias against stents. Unfortunately she needed two stents but got neither, in my mind to her detriment.
One was needed for restoration of a thrombosed jugular vein that resulted from an angioplasty about six months ago by another IR in another country.Chronic thombosis probably needs a stent in almost all situations to remain open
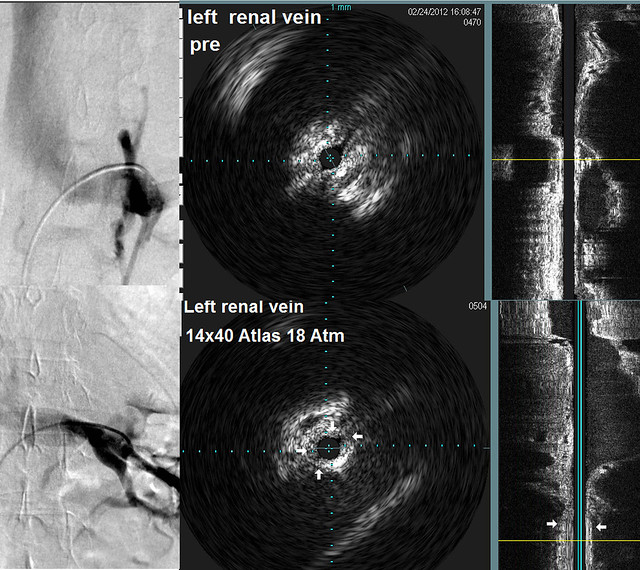
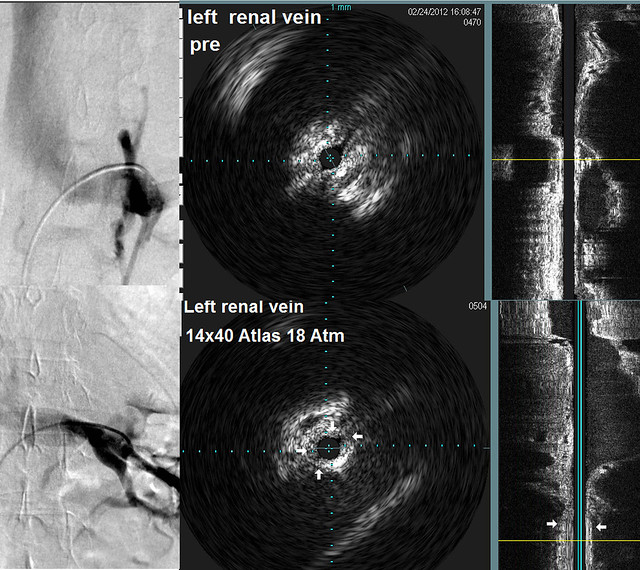
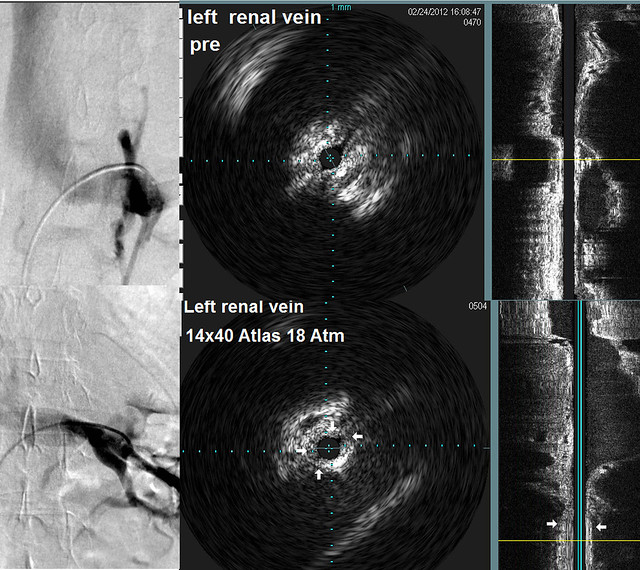
I am showing images of the Nutcracker syndrome. This obstruction augments flow into the perivertebral plexus and this can be damaging to the spine. It was alleged that dr mcguckin was advocating angioplasty alone, something i disagree with.
below you will see a nutcracker syndrome with before and after IVUS showingthat large balloon high pressure angioplasty had NO EFFECT on the obstruction.
We need to have another discussion about stents because I believe that this woman's decision was based upon fear and not on scientific evidence. There are two well recognized indications for stenting and she i think she hurt herself by her decisions
Re: Stent fears inhibit good care sometimes
Posted: Sat Feb 25, 2012 6:51 am
by HappyPoet
Oh, this is such a sad situation. When not stenting allows blood flow to continually, negatively impact the upper cerebrospinal venous flows, the patient's CCSVI-related symptoms won't resolve. You are one of the most conservative IRs regarding stents, so I know that if you say a stent is needed, a stent truly is needed.
Her spine is worrisome. lf her discs, cord or nerve roots ever become involved, she might be forced to come back real fast. With stents, combined with your vast experience, IVUS, anticoagulants, and proper follow-up ultrasounds, she could live a healthier, happier life.
Re: Stent fears inhibit good care sometimes
Posted: Sat Feb 25, 2012 7:26 am
by Cece
I remember the discussion with you prior to my second treatment in July. My renal vein had not been checked previously and you were saying that, if there was a stenosis there, stenting would be necessary. I understand CCSVI pretty well and even I was frightened at the thought of a stent. But yes a cleared thrombosis and a renal vein compression are both situations where there is no option but a stent. It is hard enough to get access to good care, to turn it down once we're there. My heart goes out to her.
Re: Stent fears inhibit good care sometimes
Posted: Sat Feb 25, 2012 8:31 am
by magoo
Dr. Sclafani,
I am scheduled to see McGuckin again on the 9th and I'm hoping he will stent the renal vein if it has collapsed again. (which it probably has, because he only used angio last time) He told me he prefers to start with angio. He said it had remained open after the ballooning. I am anxious to know what's going on in my veins since I've had a new lesion on MRI and some symptoms have returned. Was Dr. McGuckin at ISNVD? What is recovery like after a stent in this area?
Thanks.
Re: Stent fears inhibit good care sometimes
Posted: Sat Feb 25, 2012 9:35 am
by Cinna
Dr. Sclafani, I agree this is a sad situation, especially so because I was in to see you for my check up on Thursday and reported that I continue to enjoy benefits from the stenting of my renal vein in July 2011. On examination you noticed the good strength in my legs. If only the patient could have heard our conversation.
In my case, seeing your presentation about nutcracker syndrome at the Patient Day the day before my procedure as well as hearing your colleague Dr. Miller's opinion (the interventional nephrologist who popped in to the operating suite), made it easy for me to accept your decision to stent.
Magoo, I did have some discomfort in the first month and I feared that the stent may have moved--an x-ray showed it hadn't. I think my apprehension about stents didn't help. Since then it's been smooth sailing.
Re: Stent fears inhibit good care sometimes
Posted: Sat Feb 25, 2012 9:44 am
by Cece
Dr. McGuckin at ISNVD stated that he prefers angio only for primary cases, and if he is consistent with that for all the veins, that would mean angio only on the first treatment of the renal and stenting more likely to be considered on the second treatment.
http://www.thisisms.com/forum/chronic-c ... ml#p186951
Best wishes, Magoo. You have been an inspiration to many so I hope he can figure out what is going on. The renal vein might still be open. Dr. McGuckin finds a much higher percentage of renal stenoses than other IRs checking the renal are finding, so it's possible some of the stenoses he counts are very low-grade, which might meant that a stent is not going to be needed.
Re: Stent fears inhibit good care sometimes
Posted: Sat Feb 25, 2012 12:17 pm
by magoo
Thanks Cinna for relaying your experience.

Cece, it was 80% blocked, so it was a big problem.
How weird am I to be hoping for a stent?!
Re: Stent fears inhibit good care sometimes
Posted: Sat Feb 25, 2012 7:43 pm
by FLJhawk
I am fairly new to this (CCSVI) and to MS, being 56 and newly dx'd with still mild symptoms. I have schedulde CCSVI treatment in Clearwater in mid-March and after reading some of the potential problems with stenting and all, I am planning to tell my doctor that I do not want any stents. Period.
Of course, I have no idea if I have stenosed veins or how bad they might be, but Dr. S's statements make me wonder that if I am told I need a stent(s), will I be irresponsible to myself for declining? Is my concern for blood clots and such unwarranted? I have felt that I can always go back and get stenting done later, but if I really need stents, why put it off???
I know this question cannot be fully answered without knowing the actual condition of one's veins, but some of us really don't know what to do. We don't want to make things worse. We already are having to do this behind the backs of our neuros! (Kidding, somewhat.) Plus, getting stents adds significantly to the cost of the procedure!
Re: Stent fears inhibit good care sometimes
Posted: Sat Feb 25, 2012 8:50 pm
by drsclafani
magoo wrote:Dr. Sclafani,
I am scheduled to see McGuckin again on the 9th and I'm hoping he will stent the renal vein if it has collapsed again. (which it probably has, because he only used angio last time) He told me he prefers to start with angio. He said it had remained open after the ballooning. I am anxious to know what's going on in my veins since I've had a new lesion on MRI and some symptoms have returned. Was Dr. McGuckin at ISNVD? What is recovery like after a stent in this area?
Thanks.
IVUS is best to determine the degree of compression and the extent of occlusion because it gives a dross section of the diameter and shows the compression in one view. The same goes for the evaluation of the effects of treatment. You can see an example a few posts earlier.
The most serious risk of this procedure is migration of the stent. Patency is high, more than 95% percent at two years. Many patients have flank pain that can last a week or two. This is due to stretch of the vein by the stent. Oversizing of the stent is commonly done to reduce risk of migration.
Dr McGuckin was at the meeting
S
Re: Stent fears inhibit good care sometimes
Posted: Sat Feb 25, 2012 9:16 pm
by drsclafani
FLJhawk wrote:I am fairly new to this (CCSVI) and to MS, being 56 and newly dx'd with still mild symptoms. I have schedulde CCSVI treatment in Clearwater in mid-March and after reading some of the potential problems with stenting and all, I am planning to tell my doctor that I do not want any stents. Period.
Of course, I have no idea if I have stenosed veins or how bad they might be, but Dr. S's statements make me wonder that if I am told I need a stent(s), will I be irresponsible to myself for declining? Is my concern for blood clots and such unwarranted? I have felt that I can always go back and get stenting done later, but if I really need stents, why put it off???
I know this question cannot be fully answered without knowing the actual condition of one's veins, but some of us really don't know what to do. We don't want to make things worse. We already are having to do this behind the backs of our neuros! (Kidding, somewhat.) Plus, getting stents adds significantly to the cost of the procedure!
I have described five indications for stenting:
1. injury to the vein during angioplasty, such as dissections that put the vein at risk of early occlusion and thrombosis or perforations that increase risk of hemorrhage.
2. multiple recurrent stenoses over a short period of time
3. stenoses that refuse to dilate by angiolasty alone
4. after recanalization of occlusions that occured previously
5. Compression syndromes that do not respond to angioplasty, such as May thurner syndrome and Nutcracker syndrome.
It is not unreasonable to delay stenting for some indications. But the most logical thing to do is have the discussion with your doctor. Assure yourself that he has plans for such sistuations and that you agree with them. Find out how many stents he has placed in the jugular vein, the azygous vein, the common iliac vein and the left renal vein. More than 2-3% stent placement in IJV is too much Less than ten renal vein stentings is not great experience
S
Re: Stent fears inhibit good care sometimes
Posted: Sat Feb 25, 2012 9:28 pm
by drsclafani
Cece wrote:Dr. McGuckin at ISNVD stated that he prefers angio only for primary cases, and if he is consistent with that for all the veins, that would mean angio only on the first treatment of the renal and stenting more likely to be considered on the second treatment.
http://www.thisisms.com/forum/chronic-c ... ml#p186951
Best wishes, Magoo. You have been an inspiration to many so I hope he can figure out what is going on. The renal vein might still be open. Dr. McGuckin finds a much higher percentage of renal stenoses than other IRs checking the renal are finding, so it's possible some of the stenoses he counts are very low-grade, which might meant that a stent is not going to be needed.
If stenting isnt indicated, then neither is angioplasty.
my indications for stenting the renal vein include
1. greater than 90% stenosis
2. opacification of the collaterals to the spine
3. symptoms such as hypertension, proteinuria, chronic fatigue,
4. pelvic congestion syndrome or varicoceles
5. CCSVI
Re: Stent fears inhibit good care sometimes
Posted: Sun Feb 26, 2012 8:53 am
by MarkW
Hello Dr S,
My thought on risks of stents is that the risks are different above and below the heart (effect of gravity). Explaining this to patients may help.
Kind regards,
MarkW
Re: Stent fears inhibit good care sometimes
Posted: Sun Feb 26, 2012 11:10 am
by ikulo
Personally I would be more comfortable recommending stents to MS patients once we have proven the efficacy of stenting as treatment of CCSVI. The debate over the risk of any treatment is only relevant when weighed against the benefits. Since we are in the infancy of treating CCSVI syndrome and outcomes do seem to vary widely, it's premature to conclude that the risk/benefit ratio is favorable for all patients. At this point, I personally think it's too soon to recommend stents to CCSVI/MS patients. My comments are aimed only toward the CCSVI/MS discussion, as I'm not familiar with nutcrack syndrome.
I chose to not do stents, and my doctor at the time said they were not doing stents for exactly those reasons I outlined above. Personally I know of some who have well over 5 stents in their jugulars with little to show in terms of improvement. Small sample size, yes, but I think it's fair to mention the flip side of this debate since many people do make decisions about treatment based on what they read here.
Re: Stent fears inhibit good care sometimes
Posted: Sun Feb 26, 2012 3:15 pm
by Brainteaser
Dr S,
Did your stenting criteria have the support of others at ISNVD?
Re: Stent fears inhibit good care sometimes
Posted: Sun Feb 26, 2012 3:39 pm
by dc10
Hi Dr S,
I have had balloonm angioplasty with slight improvements which went awa after a few weeks post-angio.
in the last angio in May 11' i asked the dr to check my renal veins and after he said they were too tiny to dilate.
Do you think even tiny renal veins could be successfully dilated with stents?
by the way, i had 50-60% IJVs stenosis and 90% Azygous stenosis. Only the IJVs dilated three times, Azygous twice. But as each of the 3 procedures was performed by different IR i dont know if they dilated the same area in the Azygous.