Page 3 of 3
Re: Stent fears inhibit good care. Sometimes patients recons
Posted: Mon Feb 27, 2012 7:15 pm
by drsclafani
Cece wrote:I took the fact that you were getting new IVUS later this year as a sign that you weren't leaving us any time soon.
I think we've been having ridiculous fun, and you more than most, since you're on the ground figuring CCSVI out. ISNVD was too much fun and I attended via twitter and abstracts!
I am specifying the age of the post when I link to it, in case your thought process has evolved, since you are altogether entitled to evolve your thoughts on CCSVI.

Happy upcoming birthday!
A really nice birthday present was a text message at 7am on sunday morning that my patient had reconsidered the use of stents and wanted to come back for a second procedure. She was hoping it would not be too long a wait since she had to fly back to greece
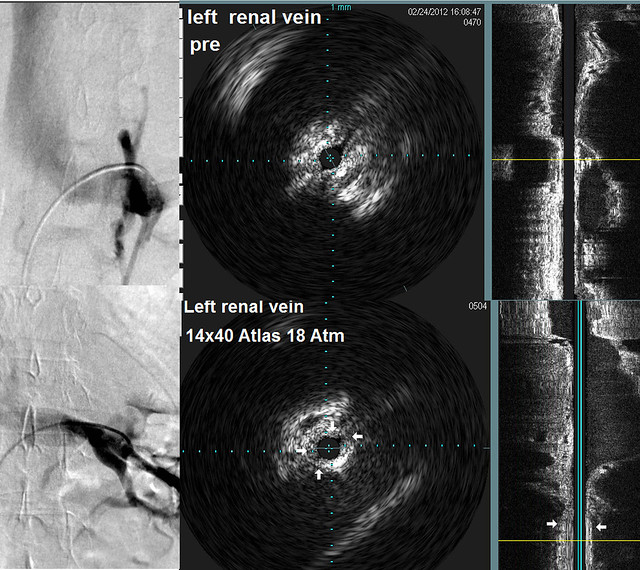
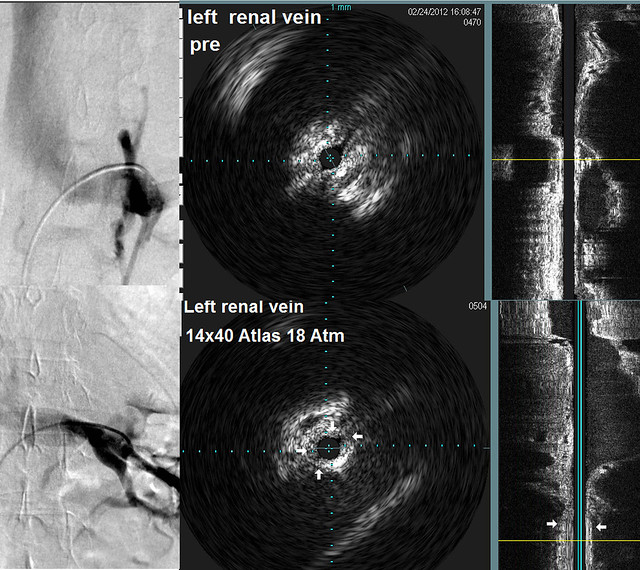
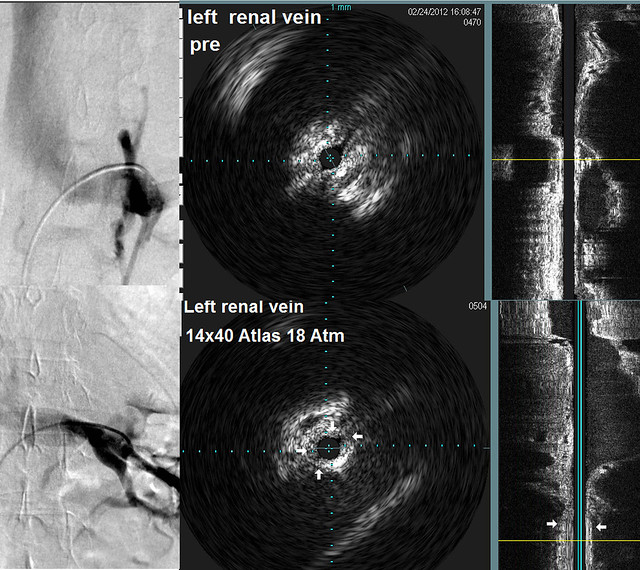
Of course i said come in monday morning and we completed the procedure today. Two stents were placed within the renal vein and flow was now excellent.

image on the left shows a large ovarian vein going into the pelvis. It is filling because its valves have been rendered incompetent by great collateral flow from the kidney .After stenting this ovarian vein is no longer opacified because blood down drains direclty into the renal vein
Re: Stent fears inhibit good care. Sometimes patients recons
Posted: Tue Feb 28, 2012 8:42 am
by Cece
drsclafani wrote:
image on the left shows a large ovarian vein going into the pelvis. It is filling because its valves have been rendered incompetent by great collateral flow from the kidney .After stenting this ovarian vein is no longer opacified because blood down drains direclty into the renal vein
Now that is unexpected and good news. What changed her mind?
From this image, it does not look like there is much redirected flow into the ascending lumbars, because it is going into the ovarian vein.
Looking back at the first image you gave us:
There we can see some contrast going up.
This also ties back in to the renal vein you showed us most recently in your thread, of the patient without MS who had been treated for pelvic vein congestion with embolization of the pelvic vein. You can see in this current case that if that ovarian vein were blocked, all that flow would redirect, most likely to the ascending lumbars and the hemiazygous and azygous vein.
Did she also consent to the stent in the thrombosed jugular, if you were able to open it? If a jugular is fully thrombosed, it makes sense that it would need a stent, because the endothelium is damaged. What if a jugular is only partially thrombosed? Does it still need a stent? If you catch a thrombosis of a jugular very quickly, can the thrombosis be cleared and no stent needed? But would that mean catching a thrombosis within a week of it thrombosing? Or how quickly?
It is preferable to prevent thrombosis, through effective anticoagulation regimen, then be trying to deal with bailout. But it was interesting that you mentioned that the greatest consensus among IRs was what to do for a bailout.
Re: Stent fears inhibit good care sometimes
Posted: Tue Feb 28, 2012 9:34 am
by dlynn
Cinna,
Did stenting your renal vein help you to walk better too? You mentioned stronger legs. I had three procedures
and my legs continue to feel weak and heavy, I never had my renal vein checked. Cinna, or anyone reading this who had benefits from
stenting or angio of the renal vein , can you please tell me your experiences and benefits?
thank you!
Re: Stent fears inhibit good care sometimes
Posted: Tue Feb 28, 2012 10:35 am
by Cinna
Dr. Sclafani, this is indeed good news. I wish her all the best.
Dlynn, yes the renal vein stent has helped me to walk better. (Like you, while my first procedure helped my gait and balance, my legs were still weak and heavy and the spasms had gotten worse)
After getting the renal stent my balance and gait improved further and I no longer have numbness in my legs when going from sitting to standing. Leg spasms are much improved and I can stand longer. Gradually I've been able to walk more, thereby strengthening my leg muscles which allows me to walk further without fatigue. As well, following an ultrasound of my legs which showed deep and superficial venous insufficiency in both legs, I started wearing compression stockings every day and I have custom orthotics. These 2 things have also helped considerably. I still have some pain in my legs and I can't walk as far as a healthy person. Occasionally, I still lose feeling in my legs and have drop foot. But after more than 20 years with MS I feel very fortunate.
Re: Stent fears inhibit good care sometimes
Posted: Tue Feb 28, 2012 10:40 am
by DougL
Cinna wrote: But after more than 20 years with MS I feel very fortunate.
yaaaaay.
Re: Stent fears inhibit good care sometimes
Posted: Tue Feb 28, 2012 3:01 pm
by dlynn
Cinna, thank you very much. Your response has helped me greatly. Tomorrow, I schedule my 4th procedure and
I'll ask my Dr. to look at the renal vein. I have a fitted leg brace that helps with strength and drop-foot.
You've answered all my questions and more, thank you again.
Re: Stent fears inhibit good care sometimes
Posted: Tue Feb 28, 2012 8:41 pm
by drsclafani
dlynn wrote:Cinna, thank you very much. Your response has helped me greatly. Tomorrow, I schedule my 4th procedure and
I'll ask my Dr. to look at the renal vein. I have a fitted leg brace that helps with strength and drop-foot.
You've answered all my questions and more, thank you again.
fourth procedure seems like a lot. when was your first procedure? I am curious to see how long your stenoses are staying open before you need another procedure. There were NO presentation about clinical experiences such as restenosis at ISNVD
thanks
s
Re: Stent fears inhibit good care. Sometimes patients recons
Posted: Tue Feb 28, 2012 8:44 pm
by drsclafani
Cece wrote:drsclafani wrote:
image on the left shows a large ovarian vein going into the pelvis. It is filling because its valves have been rendered incompetent by great collateral flow from the kidney .After stenting this ovarian vein is no longer opacified because blood down drains direclty into the renal vein
Now that is unexpected and good news. What changed her mind?
From this image, it does not look like there is much redirected flow into the ascending lumbars, because it is going into the ovarian vein.
Looking back at the first image you gave us:
There we can see some contrast going up.
This also ties back in to the renal vein you showed us most recently in your thread, of the patient without MS who had been treated for pelvic vein congestion with embolization of the pelvic vein. You can see in this current case that if that ovarian vein were blocked, all that flow would redirect, most likely to the ascending lumbars and the hemiazygous and azygous vein.
Did she also consent to the stent in the thrombosed jugular, if you were able to open it? If a jugular is fully thrombosed, it makes sense that it would need a stent, because the endothelium is damaged. What if a jugular is only partially thrombosed? Does it still need a stent? If you catch a thrombosis of a jugular very quickly, can the thrombosis be cleared and no stent needed? But would that mean catching a thrombosis within a week of it thrombosing? Or how quickly?
It is preferable to prevent thrombosis, through effective anticoagulation regimen, then be trying to deal with bailout. But it was interesting that you mentioned that the greatest consensus among IRs was what to do for a bailout.
I rely upon my excellent technologist, Smitty to save the pertinent images. He didnt understand the importance of showing those vertebral plexus opacification images so they were not available to me. But rest assured, there WERE images that showed that
s
Re: Stent fears inhibit good care. Sometimes patients recons
Posted: Wed Feb 29, 2012 10:07 am
by Cece
Aw, Smitty! We need us some vertebral plexus opacification images! (and doesn't vertebral plexus opacification roll right off the tongue...)
Smitty was there for my procedure. He was excellent and then some. Great rapport with Dr. Sclafani. Great at calming or distracting small talk before the procedure. Possibly he deserves a pay raise.
Re: Stent fears inhibit good care sometimes
Posted: Wed Feb 29, 2012 4:21 pm
by dlynn
Dr. Sclafani,
My first procedure was Jan. 2011, I had 3 really good weeks, 2nd was May, had only 2 good days, 3rd was end of june with 5 1/2 good mos.
Ultrasound showed restenosis Maybe I need stents?? (sorry I don't know how to highlight your response to my post)
dlynn
Re: Stent fears inhibit good care sometimes
Posted: Wed Feb 29, 2012 11:03 pm
by drsclafani
dlynn wrote:Dr. Sclafani,
My first procedure was Jan. 2011, I had 3 really good weeks, 2nd was May, had only 2 good days, 3rd was end of june with 5 1/2 good mos.
Ultrasound showed restenosis Maybe I need stents?? (sorry I don't know how to highlight your response to my post)
dlynn
That is odd. Three procedures is a lot in one year. But the l ast one lasted six months. Either doctor is getting better or doctor got something he or she missed on the first two procedures. But now the questions comes up about a fourth procedure with possbily stents. I would give it one more try before stents.
Re: Stent fears inhibit good care sometimes
Posted: Thu Mar 01, 2012 6:55 am
by dlynn
Dr. Sclafani,
Am I missing something? ( your last post you didn't comment) You wrote, "4th procedure seems like alot..." I agree.
Four procedures does seem like too many in a little over one year.
dlynn
Re: Stent fears inhibit good care sometimes
Posted: Thu Mar 01, 2012 8:01 pm
by dlynn
Thank you Dr. Sclafani,
My first Dr. did my first procedure, my second Dr. did the next two procedures. Could my age have something to
do with restenosis? I'm 54. He found new stenosis in my vertebral veins and my LIJV restenosed twice. Can I
safely do a fourth before I even get stents (if needed)? I have no other health issues. thank you
dlynn
Re: Stent fears inhibit good care sometimes
Posted: Mon Mar 05, 2012 1:50 pm
by Nasti
Dr. Sclafani, what are the long-term projected dangers of stents in the jugulars? What about higher in the neck? It kind of instills uncertainty within patients when some docs used to put stents and now they non-compromisingly don't!
Thnx