All the suspects in one place...
Posted: Thu Jan 10, 2013 7:47 am
Another wacky theory...
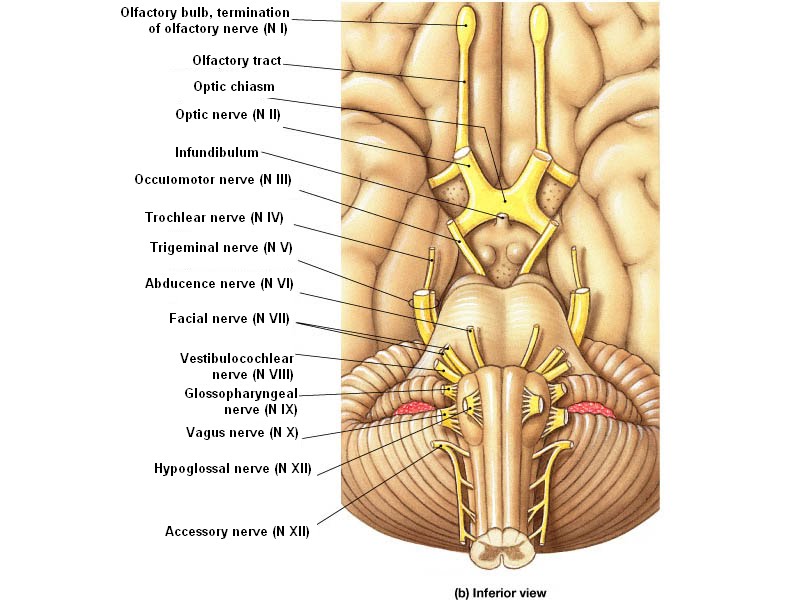
I think this is how CCSVI angioplasty and atlas realignment work. They both (sometimes) result in improvements much like those felt with use of antihypertensive drugs. They both (sometimes) result in improved autonomic function and other improvements that can be attributed to glossopharyngeal and vagus nerve decompression. The glossopharyngeal and vagus nerves meet at the entry zone of the rostral ventrolateral medulla. In many hypertensives, this area has been found to be compressed by surrounding blood vessels which could be caused/exacerbated by increased vessel pressure due to occlusion (bad valves/stenosis) and/or a misaligned atlas. Compression of this same area could cause many MS blamed issues. Angioplasty and atlas realignment can reduce this compression.
If I'm not completely off my rocker, this means we could determine whether a patient should go for angioplasty or atlas adjustment before taking any drastic measures...removing part of the experimental element. Or, if there is no compression of the area, don't do either procedure and spend your money elsewhere.
If only we could test our own theories...hehe...that could be so dangerous...especially in my numb hands.
http://hyper.ahajournals.org/content/30/1/77.full
I think this is how CCSVI angioplasty and atlas realignment work. They both (sometimes) result in improvements much like those felt with use of antihypertensive drugs. They both (sometimes) result in improved autonomic function and other improvements that can be attributed to glossopharyngeal and vagus nerve decompression. The glossopharyngeal and vagus nerves meet at the entry zone of the rostral ventrolateral medulla. In many hypertensives, this area has been found to be compressed by surrounding blood vessels which could be caused/exacerbated by increased vessel pressure due to occlusion (bad valves/stenosis) and/or a misaligned atlas. Compression of this same area could cause many MS blamed issues. Angioplasty and atlas realignment can reduce this compression.
If I'm not completely off my rocker, this means we could determine whether a patient should go for angioplasty or atlas adjustment before taking any drastic measures...removing part of the experimental element. Or, if there is no compression of the area, don't do either procedure and spend your money elsewhere.
If only we could test our own theories...hehe...that could be so dangerous...especially in my numb hands.
http://hyper.ahajournals.org/content/30/1/77.full
Neurovascular Compression of the Rostral Ventrolateral Medulla Related to Essential Hypertension
Satoshi Morimoto, Susumu Sasaki, Shigeyuki Miki, Tetsuyoshi Kawa, Hiroshi Itoh, Tetsuo Nakata, Kazuo Takeda, Masao Nakagawa, Osamu Kizu, Seiichi Furuya, Shoji Naruse, Tomoho Maeda
From the Second Department of Medicine (S. Morimoto, S.S., S. Miki, T.K., H.I., T.N., K.T., M.N.) and Department of Radiology (O.K., S.F., S.N., T.M.), Kyoto Prefectural University of Medicine, Kyoto, Japan.
Abstract
The rostral ventrolateral medulla (RVLM) is thought to serve as a final common pathway for the integration of central cardiovascular information and to be important for the mediation of central pressor responses. An association between essential hypertension and neurovascular compression of the RVLM has been reported. To confirm this relationship and to quantitatively measure the distances between the RVLM and the neighboring arteries, we performed magnetic resonance imaging using a high-resolution 512×512 matrix and magnetic resonance angiography in 49 subjects (21 patients with essential hypertension, 10 patients with secondary hypertension, and 18 normotensive subjects). One patient with essential hypertension was excluded from the evaluations because of inadequate assessment due to poor images. Neurovascular compression of the RVLM was observed in 15 of 20 (75%) patients with essential hypertension. In contrast, neurovascular compression was observed in only 1 of 10 (10%) patients with secondary hypertension and only 2 of 18 (11%) normotensive subjects. The rate of observed neurovascular compression in the essential hypertension group was significantly higher than that in the secondary hypertension group and the normotensive group (P<.01 for both). The distances between the RVLM and the nearest arteries in the essential hypertension group were significantly shorter than those in the other groups (P<.05 for all). On the other hand, the distances between the surface of the medulla oblongata and the nearest arteries did not differ among these three groups. These results suggest that neurovascular compression of the RVLM, but not of the other regions of the medulla oblongata, is particularly related to essential hypertension.
The rostral ventrolateral medulla (RVLM), a major center of the sympathetic nervous system, helps regulate the cardiovascular system.1 2 An increase in blood pressure by electrical or chemical stimulation of the RVLM and a decrease in blood pressure by chemical inhibition of the RVLM have been reported.3 4 5 6 Since the initial report by Jannetta and Gendell in 1978,7 clinical and experimental observations, including magnetic resonance imaging (MRI) studies, have indicated an association between essential hypertension and neurovascular compression of the ventrolateral medulla at the root-entry zone of glossopharyngeal and vagus nerves (ie, the RVLM).8 9 10 11 12 13 14 15 16 In the present studies, we performed MRI using a high-resolution 512×512 matrix, a new magnetic device, and magnetic resonance angiography (MRA) to obtain more precise information. We tested for an association between neurovascular compression of the RVLM and essential hypertension by evaluating the frequency of the observed neurovascular compression of the RVLM and by quantifying the distances between the surface of the RVLM and the neighboring arteries and between the surface of the medulla oblongata and the nearest arteries in patients with essential hypertension, patients with secondary hypertension, and normotensive subjects.
Case Selection
We recruited 21 patients with essential hypertension (9 women), 10 patients with secondary hypertension (3 women), and 18 normotensive subjects (7 women). The present study was approved by the ethics committee of Kyoto Prefectural University of Medicine. Informed consent was obtained from all subjects. In the secondary hypertension group, 7 patients had renal hypertension, 2 had primary aldosteronism, and 1 had pheochromocytoma. Patients older than 75 years were excluded. The mean age of the essential hypertension group was 58±12 years, that of the secondary hypertension group was 52±17 years, and that of the normotensive group was 50±14 years; age did not differ significantly among the three groups. The normotensive subjects had a systolic pressure less than 140 mm Hg and a diastolic pressure less than 90 mm Hg (118±8/67±11 mm Hg). The patients with essential hypertension and secondary hypertension were all receiving antihypertensive drugs. The duration of hypertension (144±110 and 140±130 months), blood pressure level (136±10/78±11 and 141±12/79±9 mm Hg), left ventricular mass calculated by echocardiograms17 (262±66 and 276±143 g), and hypertension stage (as determined by the extent of organ damage according to 1993 World Health Organization/International Society of Hypertension [WHO/ISH] criteria18 ) at the time of entry to this study were not significantly different between the two hypertensive groups (Table 1⇓).
Imaging Methods
MRI and MRA studies were performed with an SMT-150X imaging device (1.5 T, Shimadzu) and a multipolarization head coil. In the MRI studies, the slices were axial, parallel to the line connecting the hard palatine and the great foramen, and coronal, parallel to the fourth ventricle. Proton density–weighted fast spin echo (SE) images (repetition time [TR]/effective echo time [TE], 5000/23 milliseconds) were obtained to avoid overestimation of the distance between brain parenchyma and artery due to a partial volume effect caused by a high signal of cerebrospinal fluid. A high-resolution (0.4× 0.4 mm/pixel) 512×512 matrix was used to estimate the precise distance between brain parenchyma and artery. Slice thickness was 3 mm, and interslice gaps were covered in a second measurement. MRA studies were performed to determine the courses of the basilar artery, the bilateral vertebral arteries, and their branches three dimensionally. The 3D-time of flight (TOF) method with magnetization transfer contrast pulse was used (TR/TE/flip angle [FA], 40 ms/8 ms/16°).
Two neuroradiologists, unaware of the subjects’ medical histories, assessed all the MRI and MRA scans to determine whether there was neurovascular compression of the retro-olivary sulcus of the medulla oblongata at the level of the root-entry zone of the glossopharyngeal and vagus nerves, assumed to be the surface of the RVLM.14 The distances between the center of the retro-olivary sulcus (RVLM) and the nearest arteries and between the surface of the medulla oblongata and the nearest arteries in the axial view at the level of the root-entry zone of cranial nerves were measured. Strictly speaking, the cuts are not anatomically comparable among cases. Nonetheless, false readings due to anatomic cuts are not considered to be an important matter because the root-entry zone of the glossopharyngeal and vagus nerves lies in a small range. Borderlines of the low-intensity area (the inner lumen of the arteries) were substituted for the arterial walls because the arterial walls investigated in this study could not be determined in MRI images.
Statistical Analysis
A χ2 test was applied to determine significant differences between groups in the neurovascular compression. Fisher’s multiple range test was applied to determine the significance of differences in the distances between the center of the retro-olivary sulcus (RVLM) and the nearest arteries and between the surface of the medulla oblongata and the nearest arteries among the three groups.
Of the 49 MRI studies, only 1 patient with essential hypertension (2%) had an inadequate assessment because of poor images and was excluded from the following evaluations. Panels a and b of Fig 1⇓ show a case of essential hypertension with neurovascular compression of the left RVLM by an anterior inferior cerebellar artery. A loop of the left anterior inferior cerebellar artery compresses the left retro-olivary sulcus at the level of the root-entry zone of the glossopharyngeal and vagus nerves (RVLM). The distance between the center of the left retro-olivary sulcus (RVLM) and the left anterior inferior cerebellar artery was 0.6 mm and that between the medulla oblongata and the nearest artery was 0.0 mm in the axial view. The compressing artery could be distinguished as an anterior inferior cerebellar artery using MRA (Fig 1c⇓ and 1d⇓) and the adjacent MRI scans. Fig 2⇓ is the MRI of a normotensive subject without neurovascular compression of the RVLM. The distance between the center of the retro-olivary sulcus (RVLM) and the nearest artery was 4.9 mm and that between the medulla oblongata and the nearest artery was 2.4 mm in the axial view.
Case of a 39-year-old man with essential hypertension. A loop of the left anterior inferior cerebellar artery impinges on the left retro-olivary sulcus (rostral ventrolateral medulla [RVLM]) in the medulla oblongata. a, Axial view of magnetic resonance imaging (MRI); b, coronal view of MRI; c, coronal view of magnetic resonance angiography (MRA); and d, axial view of MRA. Ant indicates anterior; V, vertebral artery; N, root-entry zone of the glossopharyngeal nerve; A, anterior inferior cerebellar artery; Lt, left; 1, distance between the center of the left retro-olivary sulcus (RVLM) and left anterior inferior cerebellar artery; 2, distance between the surface of the medulla oblongata and anterior inferior cerebellar artery; P, posterior inferior cerebellar artery; and R, RVLM (rostral ventrolateral medulla).
Case of a 39-year-old normotensive man. No vascular structure apparently compresses the medulla oblongata. a, Axial view of magnetic resonance imaging (MRI); b, coronal view of MRI; and c, coronal view of magnetic resonance angiography. Abbreviations are as in Fig 1⇑ legend; and P, posterior inferior cerebellar artery; N, root-entry zone of the vagus nerve; 1, distance between the center of the left retro-olivary sulcus (RVLM) and posterior inferior cerebellar artery; 2, distance between the surface of the medulla oblongata and posterior inferior cerebellar artery.
Neurovascular compression of the RVLM was observed in 15 of 20 patients (75%) with essential hypertension, excluding 1 patient whose images were inadequate for assessment. In contrast, neurovascular compression was observed in only 1 of 10 patients (10%) with secondary hypertension and in only 2 of 18 normotensive subjects (11%). The rate of observed neurovascular compression in the essential hypertension group was significantly higher than that in the secondary hypertension group and normotensive group (P<.01 for both). The compressing artery was the posterior inferior cerebellar artery in 10 (67%), anterior inferior cerebellar artery in 2 (13%), and vertebral artery in 3 (20%) of 15 patients with essential hypertension. The compressing artery in 1 patient with secondary hypertension and in 2 normotensive subjects was the posterior inferior cerebellar artery. Neurovascular compression was seen on the left side in 7 and on the right side in 7 patients and on both sides in 1 of 15 patients with essential hypertension. Neurovascular compression in 1 patient with secondary hypertension and in 2 normotensive subjects was seen on the right side (Table 2⇓). Although Fig 1a⇑ might suggest neurovascular compression of the glossopharyngeal nerve, cardiopulmonary deafferentiation has not been reported to induce sustained blood pressure elevation.19 Also, no such findings were observed in the other subjects. Therefore, it is not likely that compression of this nerve contributes to the occurrence of hypertension.
Table 3⇓ shows the results of quantitative evaluations of the distances between the center of the retro-olivary sulcus (RVLM) and the nearest arteries and between the surface of the medulla oblongata and the nearest arteries. The distances between the center of the retro-olivary sulcus (RVLM) and the nearest arteries were 1.1±3.0 mm in the essential hypertension group, 4.9±4.0 mm in the secondary hypertension group, and 3.8±2.2 mm in the normotensive group. The distances in the essential hypertension group were significantly shorter than those in the secondary hypertension group and normotensive group (P<.05 for both). In contrast, the distances between the surface of the medulla oblongata and the nearest arteries were 0.5±0.9 mm in the essential hypertension group, 1.5±1.6 mm in the secondary hypertension group, and 1.6±2.1 mm in the normotensive group; there were no significant differences among the three groups. These results suggest that neurovascular compression of the RVLM, but not the other regions of the medulla oblongata, is particularly related to essential hypertension.
View this table:
In this window In a new window
Table 3.
Distances Between the Rostral Ventrolateral Medulla and Nearest Arteries
Using a new magnetic resonance device, we confirmed the association between essential hypertension and neurovascular compression of the RVLM. In addition, we found that the distances between the surface of the RVLM, but not that of the other regions of the medulla oblongata, and the neighboring arteries are significantly shorter in essential hypertension.
Jannetta et al9 noticed 2 patients with glossopharyngeal neuralgia who had hypertensive strokes after microvascular decompression of the root of the glossopharyngeal nerve in 1973. On the basis of these 2 cases, the relationship between the role of the RVLM and high blood pressure was investigated. Neurovascular compression of the RVLM was found in 51 of 53 hypertensive patients and in none of 50 normotensive patients who underwent microvascular decompression for unrelated cranial nerve dysfunction. High blood pressure returned to normal in 32 and improved in 4 of 42 patients who were treated with left microvascular decompression of the RVLM. On the other hand, blood pressure remained unchanged in the 7 hypertensive patients who were treated with right microvascular decompression of the RVLM.9 Jannetta et al10 also reported the development of hypertension by pulsatile compression on the left RVLM and normalization of the blood pressure by the cessation of the pulsatile compression in an experimental baboon model. Angiographic and pathological studies further indicated that the neurovascular compression of the left RVLM was involved in essential hypertension.12 13 14 Although two investigations of neurovascular compression using MRI have been reported,15 16 quantitative analysis of the relationship between the RVLM and the neighboring arteries had not been evaluated. In the present study, quantitative analysis of the relationship between the RVLM and the nearest arteries and between the surface of the medulla oblongata and the nearest arteries could be estimated because we used proton density–weighted images with a high-resolution 512×512 matrix.
We considered obtaining MRI images by 3D reconstruction of the ventral portion of the medulla oblongata to know the specific nature of the compression. However, it is impossible to obtain images that are fine enough to give us any information about the specific nature of the compression with a low-resolution matrix. On the other hand, to obtain MRI images by 3D reconstruction using a high-resolution 512×512 matrix, which might give us more information about the compression, we needed highly developed new software, and in theory, it might have taken much time (more than 2 hours) to perform the MRI studies. For these reasons, we did not obtain MRI images by 3D reconstruction in the present study.
The distances between the center of the retro-olivary sulcus (RVLM) and the nearest arteries in the essential hypertension group were significantly shorter than those in the secondary hypertension group and the normotensive group (P<.05 for both). On the other hand, there were no significant differences between the essential hypertension group and secondary hypertension group, or the essential hypertension group and the normotensive group, in the distances between the surface of the medulla oblongata and the nearest arteries. Because the margin of the RVLM cannot be determined in MRI studies, the existing reports using MRI could not indicate the specific relationship between the RVLM and essential hypertension. In contrast, we found that the neurovascular compression of the RVLM, but not the other regions of the medulla oblongata, may be related to essential hypertension by using MRI with a high-resolution 512×512 matrix.
Neurovascular compression of the RVLM in essential hypertension has been reported to be seen more frequently on the left side.9 11 12 13 14 15 16 However, the number of observed neurovascular compressions of the RVLM was symmetrical in the present study. Jannetta et al9 reported that blood pressure remained unchanged in seven hypertensive patients who had been treated with right microvascular decompression of the RVLM as described above. These authors hypothesized that the left side of the medulla oblongata is more sensitive to compression because the major part of the afferent inputs from the myocardial receptors of the left ventricle and atrium to the nucleus tractus solitarii is conducted by the left vagus nerve.9 20 However, cardiopulmonary deafferentiation has not been reported to induce sustained blood pressure elevation19 as described above, or the RVLM has not been reported to be functionally asymmetrical in experimental studies. Therefore, the significance of the laterality of neurovascular compression at the RVLM requires further study.
In a pathological study, Naraghi et al14 described the involved vessels and three types of neurovascular compression: type I (monovascular), caused by a single vessel loop of a branch originating from the vertebral or basilar artery, eg, the posterior inferior cerebellar artery; type II (vertebral), caused by an ectatic vertebral artery; and type III (combined), a combination of types I and II. They reported that type I was the most common type, and our result is consistent with theirs. The specific branch of the vertebral artery was difficult to determine using only MRI. MRA was thus very useful for the de- termination of the specific branch because the branches of the vertebral artery could be visualized three-dimensionally.
Prolonged hypertension causes elongated and tortuous arteries. In the present study, however, only 1 of 10 patients in the secondary hypertension group had neurovascular compression of the RVLM, whereas in the essential hypertension group, 15 of 20 patients had neurovascular compression. The duration of hypertension, left ventricular mass, and hypertension stage (as classified by the extent of organ damage according to the WHO/ISH meeting) were not significantly different between the two hypertension groups. The distances in the secondary hypertension group are rather longer than those of the normotensive group, although they are not significantly different. Thus, it is not likely that neurovascular compression of the RVLM or a shorter distance between the RVLM and the nearest artery is the natural outcome of a chronic blood pressure elevation. This finding further supports our hypothesis that neurovascular compression of the RVLM might be a cause rather than a result of high blood pressure, at least in a subgroup of patients with essential hypertension.
In summary, with the use of proton density–weighted images with a high-resolution 512×512 matrix, we found that the distances between the surface of the RVLM, but not that of the other regions of the medulla oblongata, and the neighboring arteries are significantly shorter in essential hypertension. Accordingly, we conclude that neurovascular compression of the RVLM might be at least partly associated with essential hypertension.