The stenosis was quite narrow in the innominate vein. The 3mm sheath completely obstructed the vein. But many stenoses are assymptomatic. for example in one report most of the stenoses and occlusions of dialysis related jugular stenoses were clinically occult. By this, i mean that the diagnosis was unrecognized by physical exams. there is usually no mention of neurological signs or fatigue, memory issues in the reports, which are usually described by radiologists.MikeInFlorida wrote:drsclafani wrote:I have great suspicion that a stent will be necessary to treat such a stenosis due to chemotherapy stenosis.
Dr. Sclafani, this is disconcerting.
1. How bad was the stenosis in the innominate?
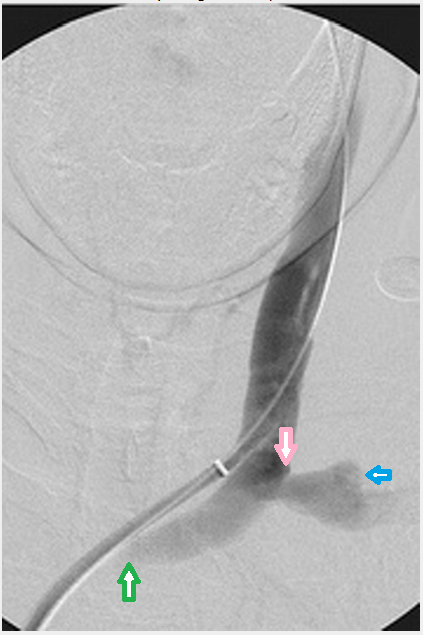
In the gurley case reports on IJV and dural sinus thrombosis, an innominate stenosis was detected in one case (does figure 11 in the paper look familiar? :Melissa B. Gurley, Teresa S. King and Fong Y. Tsai (1996) Sigmoid Sinus Thrombosis Associated with Internal Jugular Venous Occlusion: Direct Thrombolytic Treatment. Journal of Endovascular Surgery: August 1996, Vol. 3, No. 3, pp. 306-314.).
In CCSVI encounter mostly valvular stenosis, occasional hypoplasia, infrequent and J2-J3 lesions, possibly due to inflammation and compressions. In chemo stenoses, this is intimal hyperplasia and scarring.2. What are the characteristics of a chemotherapy stenosis versus the typical stenoses you encounter?
chemotherapy stenoses are actually two types: one due to the cancers themselves. these are extrinsic. Catheter induced or chemotherapy induced stenosis are thickening of the endothelium, inflammatory scar and prone to elastic recoil. I think they are more likely to develop thrombosis but could not find the reference.3. Specifically, do chemotherapy stenoses weaken the endothelial wall? Are they more delicate? More prone to thrombosis? More prone to elastic rebound?
The long term outlook for simple balloon angioplasty is not great. Most patients will require periodic dilatation. However intimal hyperplasia and compression of the stents are well known in this area. So I am inclined to see who well our patient tolerates this and a second angioplasty, and how well she responds to the angioplasty from her ccsvi symptoms. I am very comfortable with second look before making any decisions on this.4. With respect to stenting, my recollection of the general tenor your historical posts is one of great reluctance to utilize stenting. Could you please elaborate on why a chemotherapy stenosis may require a stent?
possibly. time will tell. We certainly bit off quite a lot in the first treatments, didnt we?.5. Do you believe that both the subclavian and innominate chemotherapy stenoses may require stenting?
6. Would a stent placed in the innominate be riskier than one placed in the subclavian (specifically, more prone to travel, or more dangerous if it did travel)?
Both have risk but i would think that either can be managed by stents if necessary with small risk of migration. However because the stents are larger, migration is particularly "annoying"
Surgical resection and graft interposition in the vein is an alternative. However comparisons between surgery and IR are bipolar. One study showed better results for surgery (against early experience with stenting). However a followup report from the same group showed similar results.7. Do any other options exist?