drsclafani wrote:WeWillBeatMS wrote:Dr. Sclafani,
Are the external jugular veins also tested for CCSVI? I know that they have not proven to be a regular problem but what about for the people like myself who have lost hearing in one ear? And at times even my good ear rings and pops and feels plugged like my bad one does all of the time.
WeWillBeatMS
The external jugular drains the face and scalp. I do not study these veins and i do not think these veins are the first line of action, perhaps they take on a greater potential when the internal jugular cannot be opened or has clotted off.
On Saturday i treated two patients with footdrop and weakness of the lower extremity. Both had exciting reduction in foot drop within the first day. I am ever cautious to have too much excitement on early findings. the proof isin the durability of these improvements.
ONe of the patients turned into a tour de force and I would like to share with you some unusual techniques that will hopefully make a difference.
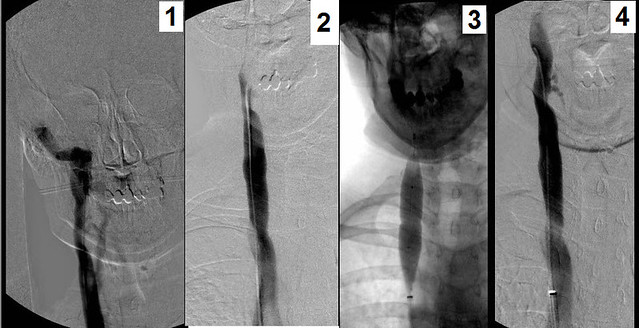
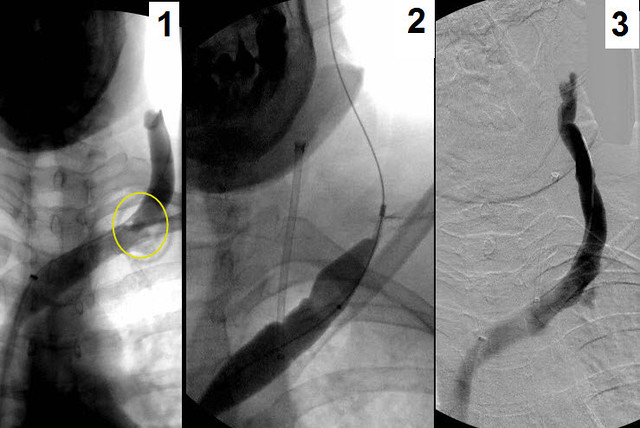
The right internal jugular vein was imaged first. The findings included clear valvular stenosis of the confluens of the IJV with the subclavian vein Figure 1, yellow circle. Simply treated by angioplasty (2), venography showed resolution of the stenosis (3)
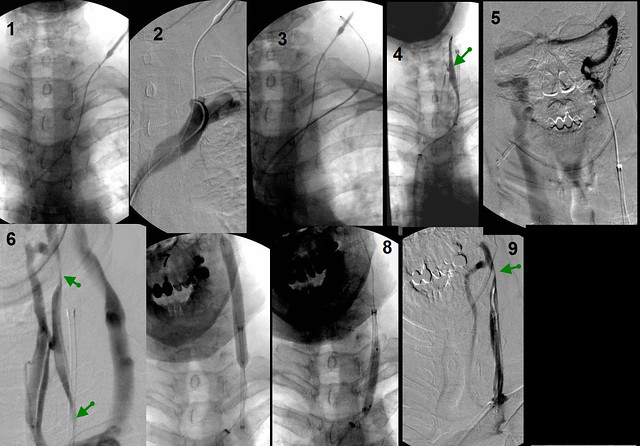
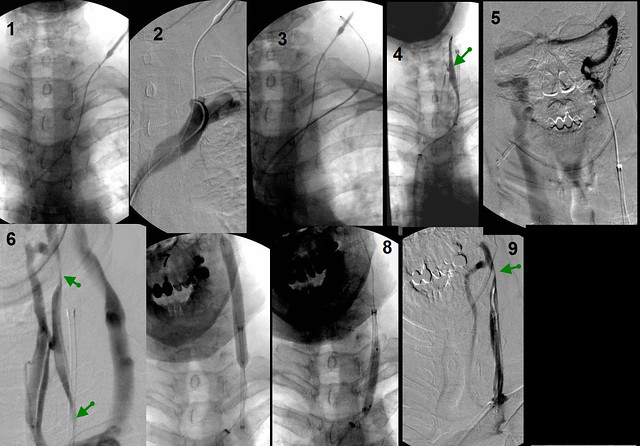
The left IJV was really prolematic and challenging. Ultrasound had shown that the vein had poor flow and was very small. As the patient had nver had angioplasty, the most likely diagnosis was hypoplasia. However recanaliation of a spontaneous occlusion was also a possibility.
After about thirty minutes of unsuccessfully trying to catheterize this vessel, i had reached my futility score.
Ultrasound of the neck was performed and I found a intermittently filled vein that was likely the IJV. So under ultrasound control, i placed a needle into the IJV. Through the needle a guidewire easilyi passed into the left inominate vein. (1). Even with the vein clearly demarkated by the jugular catheter, i could not advance the chest catheter into the jugular vein. You can see the stump of the IJV in (fig 2).
Just to make sure that the neck catheter was not in the external jugular vein, i placed the chest catheter into the external jugular vein, (3) i
The next step was to grab the chest guidewire with a snare placed through the neck sheath and pull it up above the obstruction (4). the Rendevous procedure. You can see from the figure 4, the catheter was in the IJV and some parts of it were open and others were stenotic.
That this was obstrucive cannot be denied. An injection at the skull base showed no flow going down the neck into the chest. on the contrary, all the contrast media refluxed into the dural sinuses and drained down the right jugular vein (figure 5). Pulling the catheter down and injecting contrast showed that the vein had areas of narrowing and areas of near normal size. (figure 6.)
The entire vein was angioplastied with 8 mm balloons. (fig 7-8)The final film shows a residual stenosis which remained after several dilatations. (figure 9).
So now I will place my first stent in one of my patients. it is ironic that i will have to bring my patient back for a second procedure, but when you use NO stents, you do not have much inventory on the shelf. because I use long Sheaths to introduce catheters, i need the stents are very long catheters and i just did not have one.
But that is not why i show this case. The conversation quoted by me at the top of this post was a question about doing angioplasty of the external jugular vein. I do not believe that there is any correlation with stenosis of the EXTERNAL jugular vein to improve hearing deficits in CCSVI. However i do believe there is a place for angioplasty but only rarely. When the patient has internal jugular obstruction, the external jugular can be an important collateral vein. When there is stenosis of the EJV, flow is impeded. Performing EJV angioplasty may improve collateral flowl.
See below
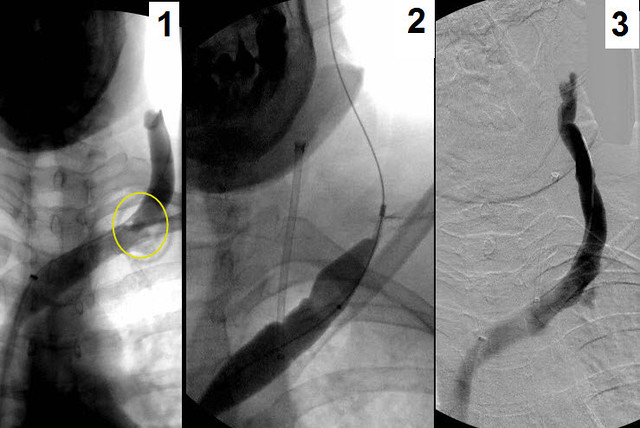
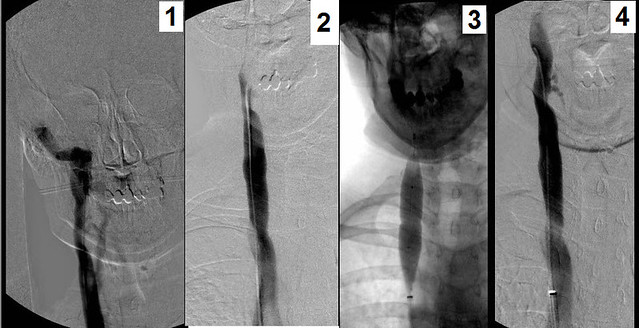
Figure 1 shows stenosis of the external jugular vein (circle).
figure 2 shows balloon angioplasty
figure 3 shows no residual stenosis in the left external jugular vein
So two first on this case, a treatment of IJV occlusion by stenting and treatment of an EJV stenosis by angioplasty.