which one indeed. NEITHER1eye wrote:If a vein is shaped like an oval it has two diameters. Which one are you using for the balloon size, or is it somewhere in between? I suppose there is a mathematical way of calculating the circumference or the radius it would have if it were round. Are you getting that finicky about it? If so, good!
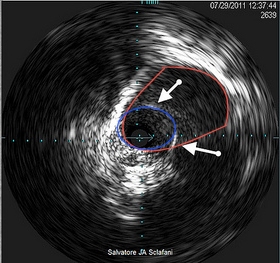
Look at the following image
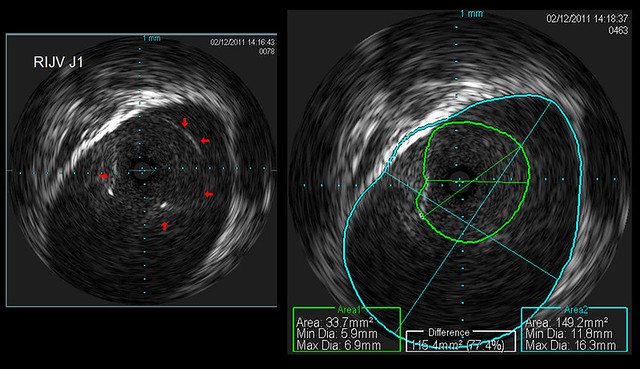
There are two colored circles. One (blue) represents the inner wall of the vein. The other (green) represents a stenotic opening of a valve. Measurements are made to the right of the vein wall (Area 2). the computer measures the shortest (11.8 mm) and the longest (16.3 mm) diameters. Above these measurements is the actual cross sectional area (149.2 mm2)
The stenotic valve had diameters of 5.9mm by 6.9mm, with a cross sectional area of 33.7 square millimeters.
So we can say that the percentage stenosis is 77%.
With the cross sectional area of the vein now known, we can calculate readily a balloon whose cross sectional area would equal or exceed that of our vein
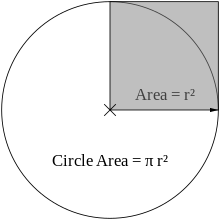
All noncompliant balloons will inflate as a circular cylinder with a cross sectional area that can be calculated by the formula cross sectional area of a circle equals Pi times the square of the radius. . It doesnt matter what the dimensions of the vein are, it will conform to the noncompliant balloon if the balloon is larger than the vein.
So calculation of each balloon based upon the known diameters give us the following table
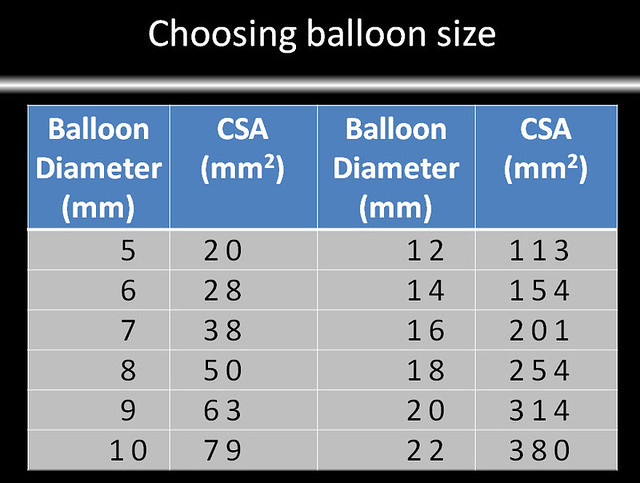
So I would choose not a 14mm balloon but would start with a 16mm balloon which has a cross sectional area about 33% larger. If the stenosis does not resolve by inflation to high pressure, I would increase the size of the balloon tgo 18mm.
the challenge will be to determine what percentage difference between the CSA of the vein and CSA of the balloon is too much or too little.