Bluesky spoke about a possibility of pelvic congestion syndrome recently. So i wanted to review this case that was performed yesterday.
The patient is a 52 year old canadian nurse with weakness and spasticity in the lower extremities, accompanied by pain, cog fog, memory issues, heat intolerance and chronic fatigue.
She had a six vessel evaluation. I am showing all the abnormal findings on venography only because of time constraints. IVUS showed that stenoses were all due to valvular immobility and stenosis.
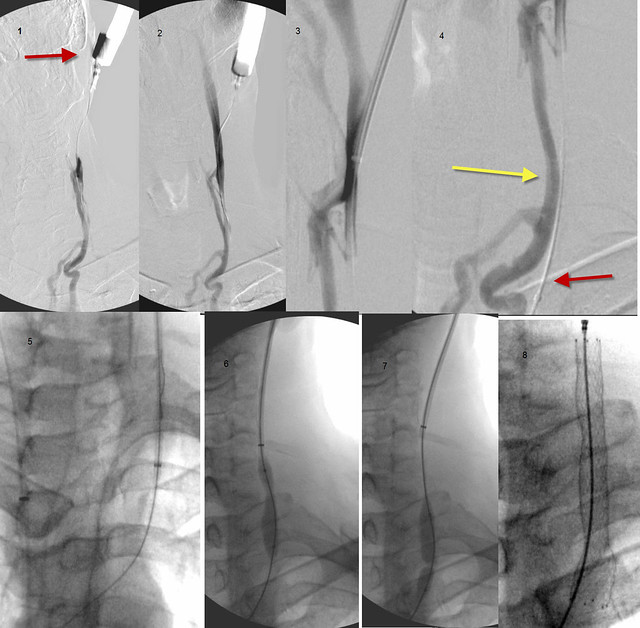
RIGHT IJV

There is a valvular stenosis at the confluens with bulging of the right sided valve cusp. 18 mm high pressure balloon used. 8 atmospheres needed to open. Results looked very good to me.
LEFT IJV
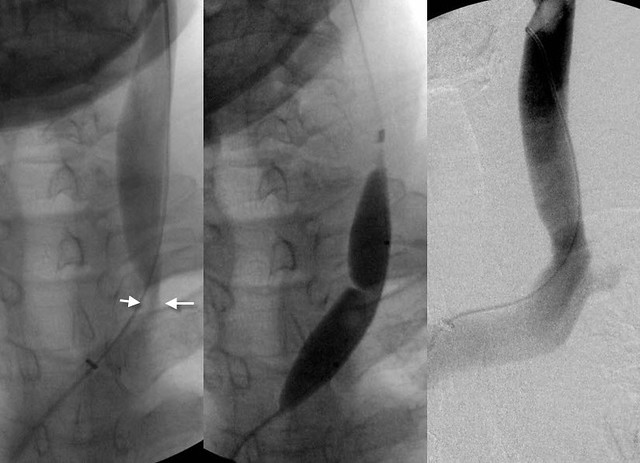
There is valvular stenosis at the confluens. Neither the cusps nor the valve leaflets were visible on venography but valve stenosis was seen on IVUS. Angioplasty with 14 mm high pressure balloon was used. Pressure was 15 Atmospheres
AZYGOUS VEIN
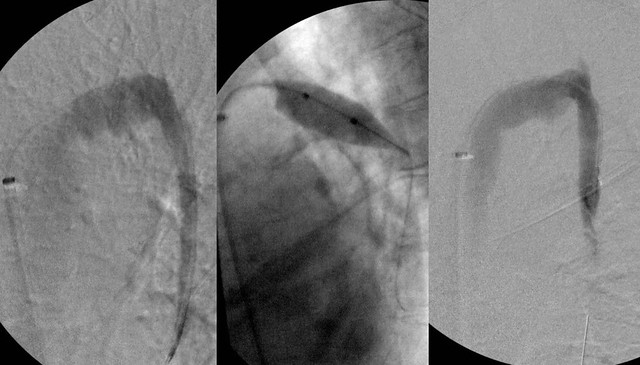
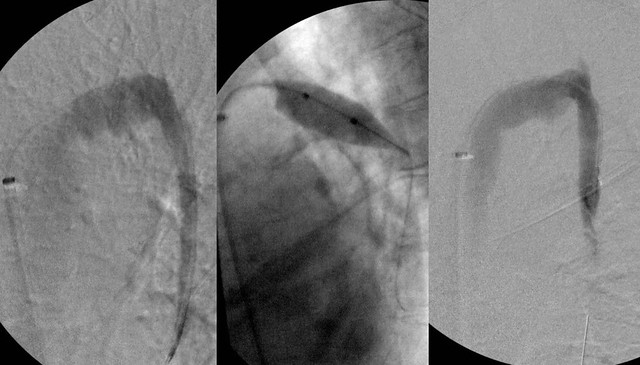
there was very high flow in the azygous vein and irregularities in the azygous arch. IVUS showed two immobile valves on the arch. A 14 mm balloon was used to 6 atmospheres with good result. IVUS showed no valve problem after treatment. But flow was very strong and the vein itself was very large, suggesting to me that we were dealing with a Nutcracker syndrome.
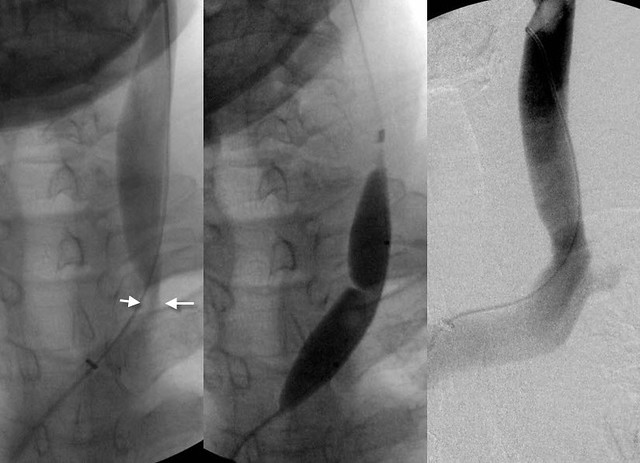
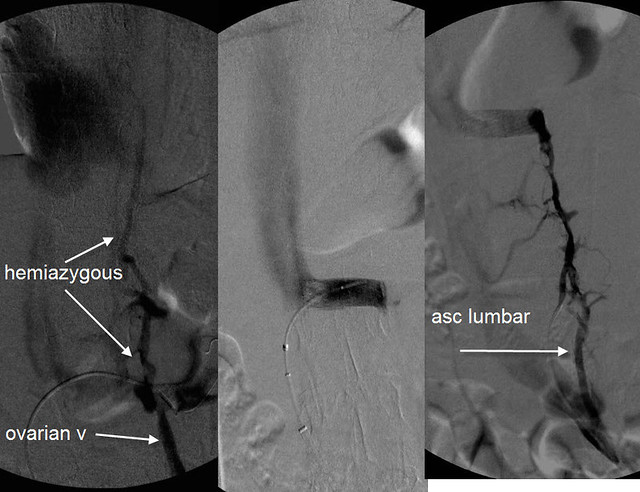
RENAL VEIN AND ASCENDING LUMBAR VEIN
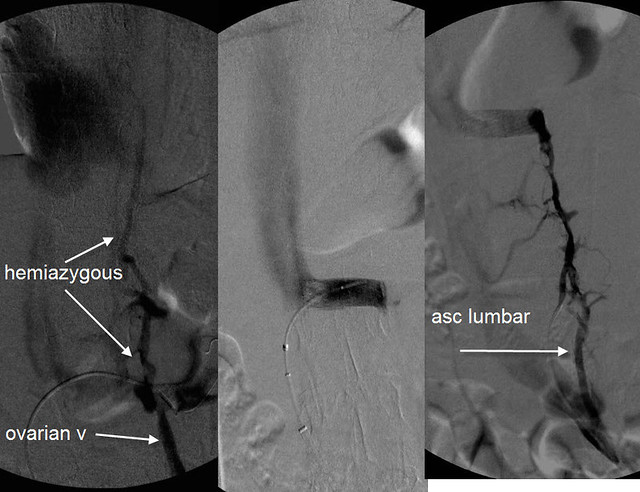
The renal venogram shows a classic Nutcracker syndrome. The contrast is "light" as the vein nears the inferior vena cava. this is caused by the compression. There is dense filling of both the ovarian vein and the hemiazygous vein which are being used as collaterals to drain the left kidney of its high blood flow volume. On the left is seen the ascending lumbar vein. this also connects to the renal vein.
RNutcracker syndrome may be a clinically occult problem in healthy patients but in patients with compromised outflow of the azygous vein, additional blood flow enters the vertebral plexus and the spinal veins. thus compounds the CCSVI resulting from the stenoses of the right and left IJV and the azygous vein.
After the competion of the procedure the patient upon questioning volunteered information regarding chronic pain near the left ovary that was, to her reminiscent of pain in the ovary during menstruation. (she is post menopausal). Thus i believe that she has pelvic congestion caused by reflux of renal vein blood into her ovarian vein resulting from the nutcracker syndrome.
It will be interesting to see whether her ovarian symptoms improve now that the renal vein has been opened. However the high flow down the ovarian vein has resulted in incompetence of the valves of her ovarian vein and she may not get relief without treatment of the ovarian vein syndromed.
The treatment is blockade of the ovarian vein from the flow in the renal vein by embolization.
Hope this is helpful bluesky
DrS