DrSclafani answers some questions
Re: DrSclafani answers some questions
Dr.S the last time I checked I wasn't a female and I update you on the 15th of every month, I be seeing you on the 16th of Feb. I gotta come see my saint.
Re: DrSclafani answers some questions
http://youtu.be/VYQRaeiOD7g
maybe it was your wife's story that made you embrace the ccsvi theory and treatment from the very start ?
maybe it was your wife's story that made you embrace the ccsvi theory and treatment from the very start ?
getafix
Re: DrSclafani answers some questions
What a great clip. I hadn't seen that one. I took notes....pelopidas wrote:http://youtu.be/VYQRaeiOD7g
maybe it was your wife's story that made you embrace the ccsvi theory and treatment from the very start ?
Questions raised in the clip:
What anticoagulation do they use?
What is the role of stents? (These IRs use stents in around 5% of the cases. Stents are on the forefront of patient's minds because of bad outcomes they've read about in forums online.)
What is the role of secondary procedures? How many procedures can or should be done on a patient? (Dr. Sclafani had a great answer, he has done a high number of secondary procedures, and they can be divided into categories: 1) Patients who, upon review of the venogram, had an incomplete procedure done the first time. No way to judge how they'll respond to secondary treatment since they weren't fully treated the first time. 2) Patients whose veins were treated very aggressively who may have sustained some insolvable damage to the veins, where nothing can be done. 3) He didn't get to the third category, although he mentioned three at the outset, and I think there must be a third? Patients who had a complete procedure the first time but restenosed? I would be in this category, and have been better since my second procedure than I was after the first.)
Is the vascular bed in CCSVI comparable to the vascular bed in dialysis patients, where procedures are repeated with frequency?
Which patients should the IRs go heroic on? Is going heroic a good thing, or is that akin to being too aggressive and the vein may be damaged (my own question there)? Who benefits more from CCSVI treatment: the patient with high disability who gets a seemingly minor improvement, such as the use of a pinky, which might enable them to operate their wheelchair and remain more independent; or a patient with low disability, who may have had less irreversible damage as suggested by Dr. Petrov? According to Dr. Siskin, older age and greater disability of a patient might incline him to treat areas he might have not treated in a younger or less disabled patient. Another option as suggested by Dr. Sclafani is to treat all other areas except the particularly challenging stenosis and see if the patient improves.
Patients are reading on forums (like ours!) about the latest techniques or ideas, which makes it important for the IRs to be in consensus.
"I don't treat multiple sclerosis. I treat CCSVI." Sal
(When IRs start talking like neurologists, they step out of their area of expertise....I like the idea of letting the neurologists tackle the neurology questions, and the IRs tackle the vascular questions....but the neurologists thus far are not particularly interested....)
In patients who are not CCSVI patients or MS patients, could the jugular approach for other procedures such as dialysis lead to brain damage? Most IRs thought not. Dr. Sclafani offered the opposing view, which is that it is worth looking into. Maybe the fatigue of dialysis patients is actually CCSVI fatigue, caused by the jugular outflow obstruction of the dialysis catheter. No way to know unless it is studied.
- drsclafani
- Family Elder
- Posts: 3182
- Joined: Fri Mar 12, 2010 3:00 pm
- Location: Brooklyn, New York
- Contact:
Re: DrSclafani answers some questions
Ms Firemsfire wrote:Dr.S the last time I checked I wasn't a female and I update you on the 15th of every month, I be seeing you on the 16th of Feb. I gotta come see my saint.
perhaps i should ask my patients to provide me with their TIMS uiisername. That way I could keep track.
For those who are unfamiliar, one of the ways i try to get detailed and continuous followup on my patients is through a monthly email. Not all do. But today I had the opportunity to do a two year followup on one of my earliest patients who is doing fabulously, despite her living in another state. I think it is possible to manage patients electronically by email and remote surrogates. It isnt easy but i am pleased to help them all regardless of where they live. I would argue that I can provide better followup this way than some patients describe with local treating docs
Noetheless, it does require time and energy and committment by both doctor and patient
Salvatore JA Sclafani MD
Patient contact: ccsviliberation@gmail.com
Patient contact: ccsviliberation@gmail.com
- drsclafani
- Family Elder
- Posts: 3182
- Joined: Fri Mar 12, 2010 3:00 pm
- Location: Brooklyn, New York
- Contact:
Re: DrSclafani answers some questions
There are a number of very personal reasons why i became committed to the CCSVI discovery, .Leading the charge to have my wife's jugular vein ligated was surely cavalier, but at the time, no one knew any better. Perhaps it is true that involvement in ccsvi is my redemption. A dear friend in a personal triangle did develop MS and perhaps this is also part of redemption and renewal.pelopidas wrote:http://youtu.be/VYQRaeiOD7g
maybe it was your wife's story that made you embrace the ccsvi theory and treatment from the very start ?
But i really think that my committment came when I met my first patient, saw the desperate hopes and needs. How could i, a healer, possibly turn my back on that.
Salvatore JA Sclafani MD
Patient contact: ccsviliberation@gmail.com
Patient contact: ccsviliberation@gmail.com
- drsclafani
- Family Elder
- Posts: 3182
- Joined: Fri Mar 12, 2010 3:00 pm
- Location: Brooklyn, New York
- Contact:
Re: DrSclafani answers some questions
too variable and without clear mandate to any one technique. personally, i think aspirin is insufficient. I use an anticoagulant for about six months. I am not sure if i should continue for longerCece wrote:What a great clip. I hadn't seen that one. I took notes....pelopidas wrote:http://youtu.be/VYQRaeiOD7g
maybe it was your wife's story that made you embrace the ccsvi theory and treatment from the very start ?
Questions raised in the clip:
What anticoagulation do they use?
i have long been negative on stents because intimal hyperplasia, thrombosis and migration are concerns but i think that the solutions are the same as with angioplasty. Sizing makes a real difference. Since I have used IVUS to size veins, the few stents i have placed are doing quite well. I think it is all about sizing and anticoagulation.What is the role of stents? (These IRs use stents in around 5% of the cases. Stents are on the forefront of patient's minds because of bad outcomes they've read about in forums online.)
Dear patients, the third category are those who were treated by me and have recurrent stenosis. This is definitely the smallest of the three groups for i have treated more patients treated elsewhere than have come to me for their first procedure. These patients Arte sust starting to come back to me after a year. Having had good results and some are starting to have frecurrent symptoms 8-12 months later. If their CCSVI ultrasound shows reflux and they have recurrent symptoms, i encourage them to undergo another treatment. If their ultrasound shows CCSVI but they are asymptomatic we put our heads together and make a plan. Generally, i do not want to treat patients who do not have major symptoms. But if they feel that their symptoms are diminishing their quality of life, i emphatically encourage them to have another procedure. To date, these patients have recurrent valvular restenoses, not strictures caused by angioplasty. I strongly believe that the vein adjacent to the angioplasty does not get injured very easily because most angioplasties have underdilated the jugular vein.What is the role of secondary procedures? How many procedures can or should be done on a patient? (Dr. Sclafani had a great answer, he has done a high number of secondary procedures, and they can be divided into categories: 1) Patients who, upon review of the venogram, had an incomplete procedure done the first time. No way to judge how they'll respond to secondary treatment since they weren't fully treated the first time. 2) Patients whose veins were treated very aggressively who may have sustained some insolvable damage to the veins, where nothing can be done. 3) He didn't get to the third category, although he mentioned three at the outset, and I think there must be a third? Patients who had a complete procedure the first time but restenosed? I would be in this category, and have been better since my second procedure than I was after the first.)
i would say emphatically NO. Dialysis stenoses are the result of the shear forces of high pressure arteries going into low pressure veins resulting in intimal hyperplasia. That just isnt the problem in ccsvi. Also the high pressure arterial flow results in continuous high flow and until intimal hyperplasia or other stenoses occur, slow flow is not the problem that we see in internal jugular veins.Is the vascular bed in CCSVI comparable to the vascular bed in dialysis patients, where procedures are repeated with frequency?
Cece, I believe we should be heroic without recklessness on every patient. One person's pinkie is another persons vision or heat intolerance. I do not think we should have to make such distincitions and we dont. My goal in that video was to champion those who were at risk for being left behind because their disease was too extensive where results might be less exciting that those younger patients with less symptoms.Which patients should the IRs go heroic on? Is going heroic a good thing, or is that akin to being too aggressive and the vein may be damaged (my own question there)? Who benefits more from CCSVI treatment: the patient with high disability who gets a seemingly minor improvement, such as the use of a pinky, which might enable them to operate their wheelchair and remain more independent; or a patient with low disability, who may have had less irreversible damage as suggested by Dr. Petrov? According to Dr. Siskin, older age and greater disability of a patient might incline him to treat areas he might have not treated in a younger or less disabled patient. Another option as suggested by Dr. Sclafani is to treat all other areas except the particularly challenging stenosis and see if the patient improves.
I do not think we will be there for some time. there are not enough patients or data yet.Patients are reading on forums (like ours!) about the latest techniques or ideas, which makes it important for the IRs to be in consensus.
it is now part of my disclosure before I lecture."I don't treat multiple sclerosis. I treat CCSVI." Sal
(When IRs start talking like neurologists, they step out of their area of expertise....I like the idea of letting the neurologists tackle the neurology questions, and the IRs tackle the vascular questions....but the neurologists thus far are not particularly interested....)
There are some neurologists who are interested and we embrace and encourage them. But it is iincorrect to suggest that those who are not neurologists who can learn and have opinions. Look at your patients!!! The void will be filled by those who go there
I now do a complete neurological examination as part of my assessment. Before my first treatment in 2009, I could not do that. Everyone can learn new things.
everything is worth looking intoIn patients who are not CCSVI patients or MS patients, could the jugular approach for other procedures such as dialysis lead to brain damage? Most IRs thought not. Dr. Sclafani offered the opposing view, which is that it is worth looking into. Maybe the fatigue of dialysis patients is actually CCSVI fatigue, caused by the jugular outflow obstruction of the dialysis catheter. No way to know unless it is studied.
Salvatore JA Sclafani MD
Patient contact: ccsviliberation@gmail.com
Patient contact: ccsviliberation@gmail.com
- drsclafani
- Family Elder
- Posts: 3182
- Joined: Fri Mar 12, 2010 3:00 pm
- Location: Brooklyn, New York
- Contact:
Re: DrSclafani answers some questions
Mark, it's on the internet. it is open information. It would great but not a mandate that the Sclafani techniqueMarkW wrote:Hello Dr S,
Is it OK for me to share this chart with NICE in UK ?
Thanks
MarkW
but most important to me is that the idea is explored, works accepted and embraced.
Salvatore JA Sclafani MD
Patient contact: ccsviliberation@gmail.com
Patient contact: ccsviliberation@gmail.com
- drsclafani
- Family Elder
- Posts: 3182
- Joined: Fri Mar 12, 2010 3:00 pm
- Location: Brooklyn, New York
- Contact:
Re: DrSclafani answers some questions
sorry, i just needed time to enjoy the weekend.Cece wrote:I would not have predicted success on the eleventh try!drsclafani wrote:Cece, i do not sweat the larger size WHEN it is necessary. This particular patient had venoplasty on the right side with an 18 mm balloon. IVUS showed that anything less on the right would have been suboptimal to me.
On the other hand, IVUS showed that 14 mm was optimal on the left side and i was loath to, but tempted, to use a 16mm when ten inflations were unsuccessful. However we got lucky and dilatation was successful on the eleventh inflation
S
In the past we've discussed the very long inflations, and that this might cut off oxygen to the vein wall itself. So I am guessing these were eleven inflations of relatively short or medium durations, so as not to hurt the vein. A longer duration of inflation might've made for a successful dilatation in fewer inflations but at the risk of oxygen deprivation to the vein walls or even thrombus forming above the balloon during extended ballooning? What I always keep coming back to is that there is a lot to the techniques of the procedure, and that it needs to be optimized, and even then it must be proven that it is optimized, and standardized! Not an easy task.
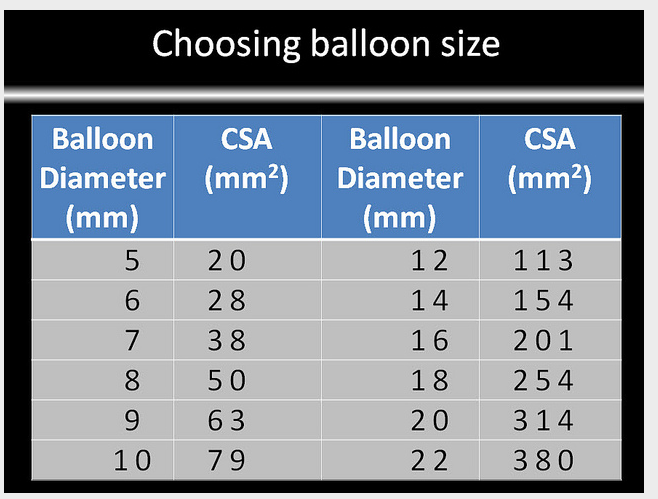
The chart for sizing by IVUS:
 Such a tease....But since i h ave been performing dural sinography, it is clear that they are very often condylar collaterals. I will try to post one today here and on my facebook page.
Such a tease....But since i h ave been performing dural sinography, it is clear that they are very often condylar collaterals. I will try to post one today here and on my facebook page.
Salvatore JA Sclafani MD
Patient contact: ccsviliberation@gmail.com
Patient contact: ccsviliberation@gmail.com
Re: DrSclafani answers some questions
I would hope all your weekends are excellent and enjoyed!
Ah! Here is the word in context, with an orangutuan picture to boot.
http://www.hwbf.org/ota/s2k/cases/sjas1.htm
Dr. Sullivan mentioned in the clip that he had a patient with a late thrombosis occur at about 3 months, and after that he extended how long he anticoagulated patients.drsclafani wrote:too variable and without clear mandate to any one technique. personally, i think aspirin is insufficient. I use an anticoagulant for about six months. I am not sure if i should continue for longerCece wrote:Questions raised in the clip:
What anticoagulation do they use?
This is good news and so is this:Since I have used IVUS to size veins, the few stents i have placed are doing quite well. I think it is all about sizing and anticoagulation.
I strongly believe that the vein adjacent to the angioplasty does not get injured very easily because most angioplasties have underdilated the jugular vein.
Half of understanding 'Dr. Sclafani Answers Some Questions' has been about getting the vocab terms straight. Going heroic is a confusing one, because yes, it is what every patient deserves, yet it is hard to think of heroic as an everyday occurrence. Is using IVUS going heroic? Is checking the renal vein going heroic? What DougL describes, with an azygous vein that was blocked and obstinate, and an IR that was more obstinate (in a good way), and a five-hour procedure, that is surely going heroic.Cece, I believe we should be heroic without recklessness on every patient. One person's pinkie is another persons vision or heat intolerance. I do not think we should have to make such distincitions and we dont. My goal in that video was to champion those who were at risk for being left behind because their disease was too extensive where results might be less exciting that those younger patients with less symptoms.
Ah! Here is the word in context, with an orangutuan picture to boot.
http://www.hwbf.org/ota/s2k/cases/sjas1.htm
The void will be filled by those who go there. I like the sound of that.There are some neurologists who are interested and we embrace and encourage them. But it is iincorrect to suggest that those who are not neurologists who can learn and have opinions. Look at your patients!!! The void will be filled by those who go there
I now do a complete neurological examination as part of my assessment. Before my first treatment in 2009, I could not do that. Everyone can learn new things.
- drsclafani
- Family Elder
- Posts: 3182
- Joined: Fri Mar 12, 2010 3:00 pm
- Location: Brooklyn, New York
- Contact:
Re: DrSclafani answers some questions
My goodness, where did you find that case. Truly one of a kind.Cece wrote:I would hope all your weekends are excellent and enjoyed!Dr. Sullivan mentioned in the clip that he had a patient with a late thrombosis occur at about 3 months, and after that he extended how long he anticoagulated patients.drsclafani wrote:too variable and without clear mandate to any one technique. personally, i think aspirin is insufficient. I use an anticoagulant for about six months. I am not sure if i should continue for longerCece wrote:Questions raised in the clip:
What anticoagulation do they use?
This is good news and so is this:Since I have used IVUS to size veins, the few stents i have placed are doing quite well. I think it is all about sizing and anticoagulation.I strongly believe that the vein adjacent to the angioplasty does not get injured very easily because most angioplasties have underdilated the jugular vein.Half of understanding 'Dr. Sclafani Answers Some Questions' has been about getting the vocab terms straight. Going heroic is a confusing one, because yes, it is what every patient deserves, yet it is hard to think of heroic as an everyday occurrence. Is using IVUS going heroic? Is checking the renal vein going heroic? What DougL describes, with an azygous vein that was blocked and obstinate, and an IR that was more obstinate (in a good way), and a five-hour procedure, that is surely going heroic.Cece, I believe we should be heroic without recklessness on every patient. One person's pinkie is another persons vision or heat intolerance. I do not think we should have to make such distincitions and we dont. My goal in that video was to champion those who were at risk for being left behind because their disease was too extensive where results might be less exciting that those younger patients with less symptoms.
Ah! Here is the word in context, with an orangutuan picture to boot.
http://www.hwbf.org/ota/s2k/cases/sjas1.htmThe void will be filled by those who go there. I like the sound of that.There are some neurologists who are interested and we embrace and encourage them. But it is iincorrect to suggest that those who are not neurologists who can learn and have opinions. Look at your patients!!! The void will be filled by those who go there
I now do a complete neurological examination as part of my assessment. Before my first treatment in 2009, I could not do that. Everyone can learn new things.
I am missing the trauma arena at this moment. How viscerally exciting it was!
Salvatore JA Sclafani MD
Patient contact: ccsviliberation@gmail.com
Patient contact: ccsviliberation@gmail.com
Re: DrSclafani answers some questions
(For anyone else reading the case, as you can see it's nothing to do with CCSVI, but a pelvic injury case, where every time the good doctor unclamped the vein he was working on, the patient bled and needed resuscitation.)
A person doesn't do trauma care for decades unless they like it, and in your case, are good at it....
But a trauma patient's trauma occurs very quickly; there has not been a length of suffering there. A CCSVI patient has a length of suffering that could be years or decades. What a gift to be able to make an impact on such suffering. What a gift too to contribute to the development of how CCSVI will be treated.
Re: DrSclafani answers some questions
Cece we have never chatted, but I could not agree with you more.
-
newlywed4ever
- Family Elder
- Posts: 255
- Joined: Thu Apr 17, 2008 2:00 pm
- Location: Michigan
- Contact:
Re: DrSclafani answers some questions
Exactly! and thank you, Cece - you say it well. One year ago I was in Brooklyn and happy angioversary to you, tooCece wrote:The case is one of the first returns in a search on "heroic technique interventional radiology."
(For anyone else reading the case, as you can see it's nothing to do with CCSVI, but a pelvic injury case, where every time the good doctor unclamped the vein he was working on, the patient bled and needed resuscitation.)
A person doesn't do trauma care for decades unless they like it, and in your case, are good at it....
But a trauma patient's trauma occurs very quickly; there has not been a length of suffering there. A CCSVI patient has a length of suffering that could be years or decades. What a gift to be able to make an impact on such suffering. What a gift too to contribute to the development of how CCSVI will be treated.
Re: DrSclafani answers some questions
Dr Sclafani, a few days ago on a different thread you made the above statement which would be very interesting and of value if you've been looking for stenosis using angiography on a significant number of people who don't have MS. What kind of with MS/without MS numbers are you talking about in that 2 year time frame?drsclafani wrote:It's nearly always positive when you go to brooklyn too. Only 1 PwMS had all veins normal in two years with use of IVUS. ONLY NEGATIVES HAVE BEEN PATIENTS UNDERGOING ANGIOGRAPHY.WITHOUT A DIAGNOSIS OF MS.
- drsclafani
- Family Elder
- Posts: 3182
- Joined: Fri Mar 12, 2010 3:00 pm
- Location: Brooklyn, New York
- Contact:
Re: DrSclafani answers some questions
LyonLyon wrote:Dr Sclafani, a few days ago on a different thread you made the above statement which would be very interesting and of value if you've been looking for stenosis using angiography on a significant number of people who don't have MS. What kind of with MS/without MS numbers are you talking about in that 2 year time frame?drsclafani wrote:It's nearly always positive when you go to brooklyn too. Only 1 PwMS had all veins normal in two years with use of IVUS. ONLY NEGATIVES HAVE BEEN PATIENTS UNDERGOING ANGIOGRAPHY.WITHOUT A DIAGNOSIS OF MS.
I do not perform angiography on normal patients any longer. I did perform many angiograms of the the carotid and jugular systems when I was doing trauma imaging of young otherwise healthy black males who had sustained gunshot wounds of the neck, face and head. Several hundred. These patients never had the appearances we see when studying patients with MS looking for venous outflow obstructions. I have in the past two years imaged a few patients who did not have a diagnosis of MS but had typical symptoms of ccsvi, namely cog fog, headaches, imbalance, memory issues, fatigue. They DID have venographic findings consistent with ccsvi. I have a couple of patients with Lymes disease, and two others who had other neurological diseases (both demyelinating but neither MS). These did not have venographic features of ccsvi.
So the number of patients without MS in the past two years is quite small. They account for less than 2%
I think i really mangled my statements .
DrS
Salvatore JA Sclafani MD
Patient contact: ccsviliberation@gmail.com
Patient contact: ccsviliberation@gmail.com
-
- Similar Topics
- Replies
- Views
- Last post
