Here are the images.drsclafani wrote:interesting case. I will show the images as soon as they are ready.....
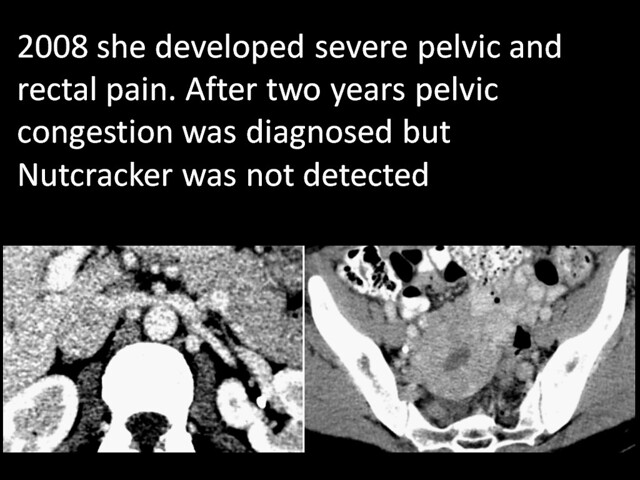
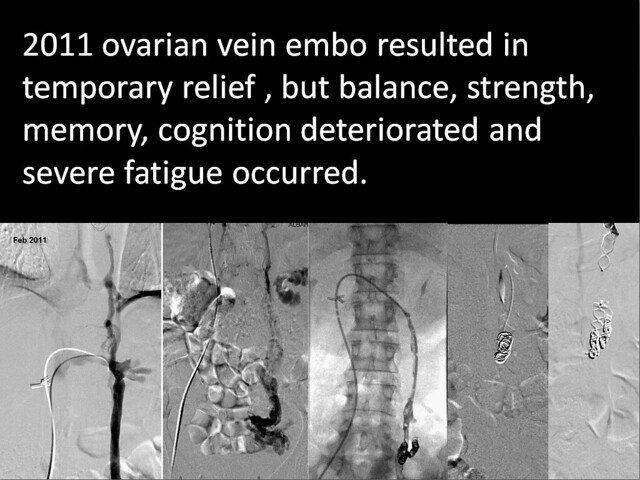
a 47 year old female college professor who was well until four years ago when she began to develop pelvic and rectal pain. After numerous and prolonged testing, she underwent gonadal venography that confirmed the presence of ovarian vein incompetence and varicosities. Pelvic congestion was manifested as well. The ovarian vein was treated by coil and Amplatzer embolization by another interventionalist. Clinical improvements in the pain were short lived. She also began to notice reduced memory, word and name recall and difficulties with multitasking and complex thinking. Balance deteriorated, severe fatigue developed and she became weak in both left upper and lower extremities. Further angiography resulted in coil embolization of the internal iliac vein. Additionally, compression of the left renal vein was identified and a diagnosis of Nutcracker syndrome was made. This was not treated.
She continued to have some relief from the pelvic pain but her new neurological symptoms worsened considerably, resulting in a subjectively diminished quality of life. She sought my consultation, having never seen a neurologist for her problems.
She gave a history of mitral prolapse with mitral regurgitation and unstable knee and poor wound healing. There was no history of multiple sclerosis, optic neuritis or vision disturbance. On physical exam she had a prominent periobital vein, hyperemia of the pharynx, drooping eyelids and double folds in her upper eyelids.She had very lax ligaments in her hands. There was slight weakness in the left hand and the left hip flexor
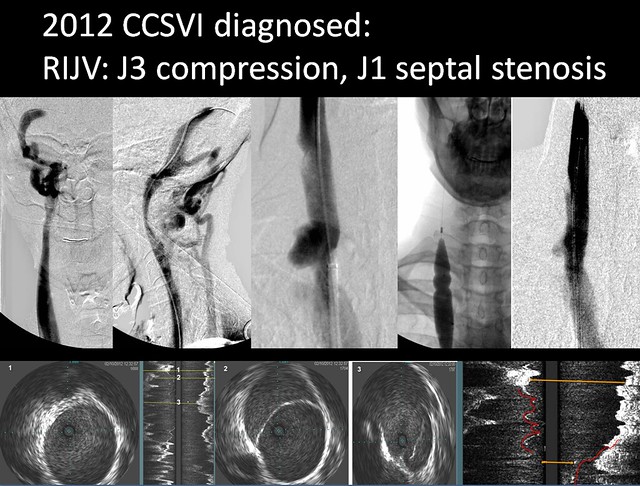
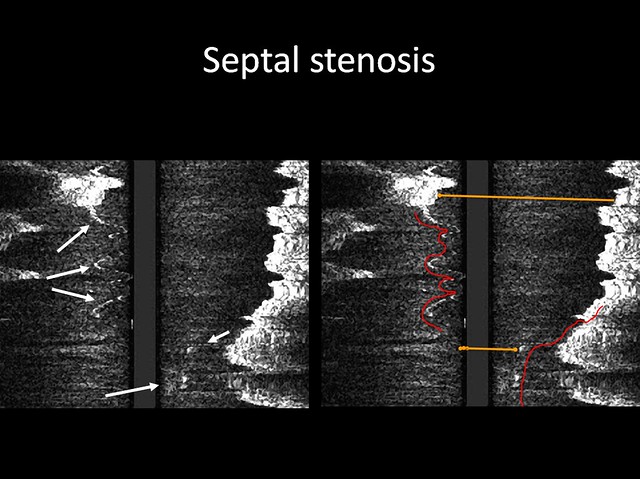
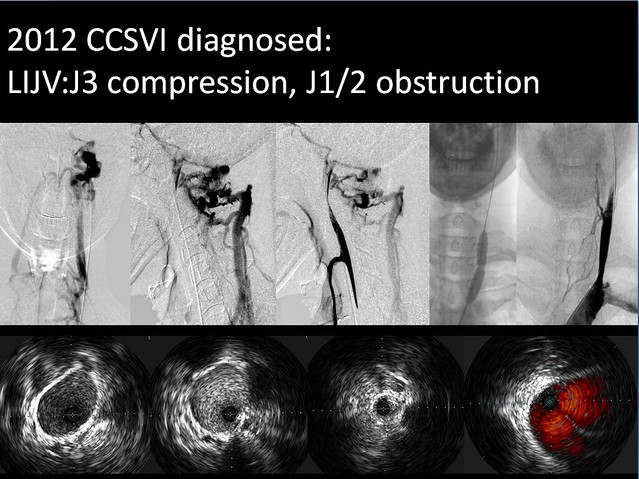
She had a CCSVI protocol neck ultrasound confirmed the presence of two criteria of CCSVI and revealed bilateral IJV reflux in both supine and erect positions in a small left internal jugular vein and a normal right internal jugular vein with a septum creating a infundibulum.
Venography and IVUS confirmed the right jugular vein (IJV) septum and demonstrated a 99% stenosis of the left IJV. Angioplasty of both IJV was performed with satisfactory but not complete dilatation on the left side. The azygous vein was enlarged and there was reflux in the accessory azygous vein.
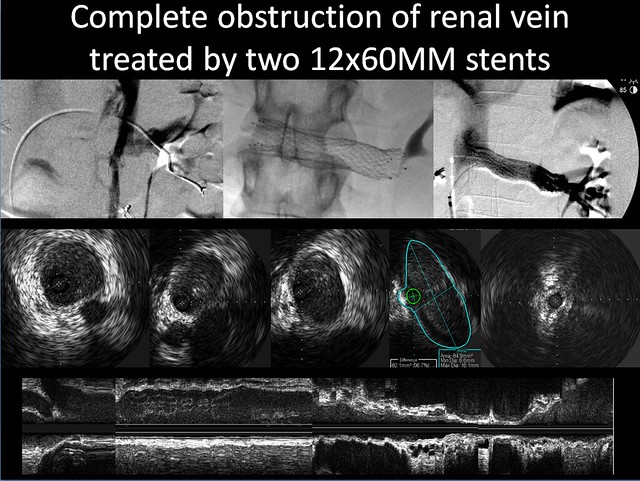
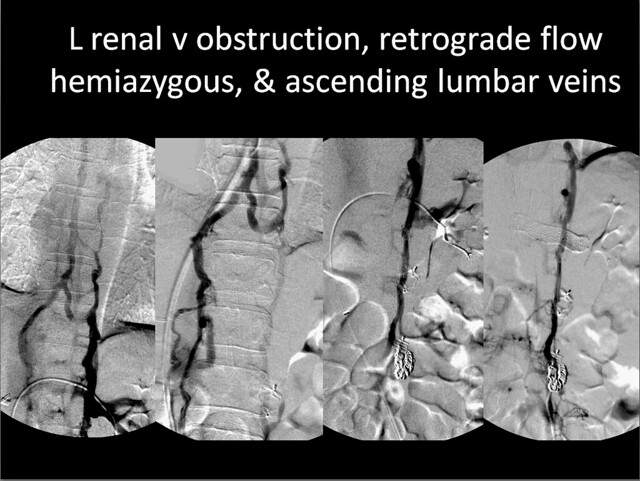
Renal venography showed a classical appearance of the nutcracker. It was very difficult to advance the guidewire or catheter through the obstructed segment that was located at the position of the aorta. Venography revealed total obstruction of the vein. There were no gonadal collaterals but there was complete opacification of the entire vertebral venous system.from T3 to L5. IVUS showed complete compressive obstruction of the vein. After self-expanded stenting between the renal bifurcation and the inferior vena cava, renal blood flow was brisk and the collaterals were no longer seen.
Within 90 minutes she stated that all pelvic pain had resolved and that she felt more alert and clear.
This interesting case shows that in the presence of CCSVI, Nutcracker Syndrome is capable of exacerbating or causing neurological symptoms. With the gonadal veins occluded by coils, renal hemodynamic redirection into the hemiazygous and ascending lumbar veins augmented flow into an already compromised cerebrospinal venous system. The effects were deficits is memory and cognition, balance, strength and the development of a severe fatigue syndrome.
Upon further assessment, Ehlers Danlos syndrome also seems like a real possibility. Do you think these patients are more prone to thrombosis or delayed endothelialization? Should I continue my anticoagulation regimen for an additional few months beyond the standard one month of antithrombin a medications?
I will send on the images as soon as they are ready.
Any questions?
DrSclafani

