It has taken me almost one week to recover from a particularly stressful, exhausting and challenging week of CCSVI treatments.
Going to three patients per day has always been fraught with the risk of more than one patient requiring more than three hours of work. Last week, the first patient one day was right on target, taking two hours and five minutes to complete a moderately complicated but uneventful procedure. Unfortunately a three hour procedure was followed by a four hour procedure. Thus a day that began at 630am with a 700am arrival at the center left with me closing the door 935pm and arriving home at 10pm.
The day before was not quite as bad but required that i drive a poor man to his hotel. You see, he did not follow instructions and came from North Carolina alone without an escort. Policy at the center, and standard of care in most ambulatory procedure centers, requires that those who have procedures be escorted home. Well, that left two choices: send him back to North Carolina (out of the question) or be his escort back to his hotel. Yes, DrS enjoyed his new role as driver. Unfortunately, the patient chose a hotel that was out of the way and was not the usual five minute drive from the doctor's house to patient's hotel. GRRRR
It was that kind of week.
The case of the week was challenging on many fronts: diagnostics, treatment options, unusual associations, to name a few. It was a great teaching and learning experience.
The patient is a 53 year old female with relapsing remitting MS first diagnosed in 1986 after headaches and visual complaints. She has had a slow steady downhill course. Among her current complaints are short term memory loss, problems with concentration and multitasking and severe fatigue. She has double vision, numbness in her fingers, weakness in her hands and legs and heat intolerance that makes her weaker. She is mobilizes by wheelchair. She has urinary frequency. She is on copaxone, ritalin and many supplements. She denies spasticity.
In August 2010 she was treated by angioplasty by an established American Group practice by angioplasty of the jugular veins. She immediately improved. Notably her vision was "perfect". Sadly, the improvement only lasted two weeks. At the current time she has chief complaints of severe overwhelming fatigue and balance problems. Ultrasound was interpreted as bilateral internal jugular vein reflux and elongated valves.
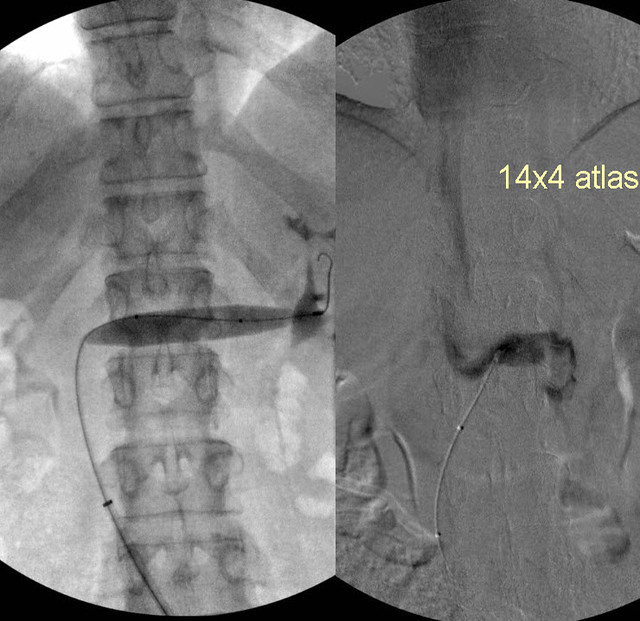
Venography was performed.
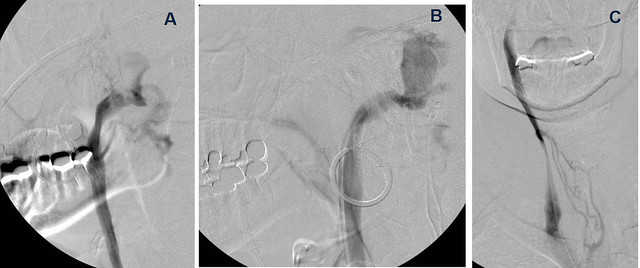
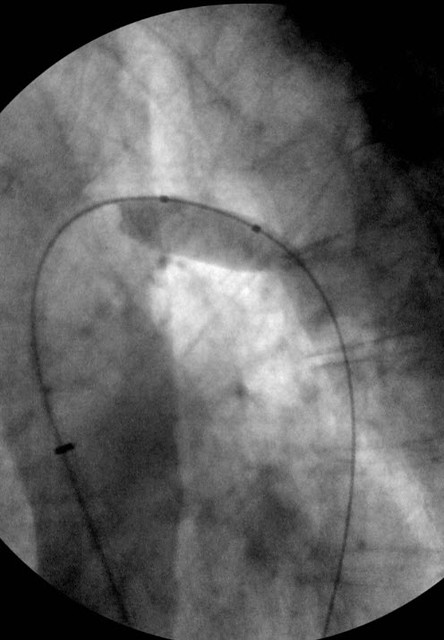
The exam began with right IJV and sigmoid sinus venography
On this image one sees the right sigmoid sinus entering the jugular bulb and draining through the jugular vein (A&B). There is good flow through the dural sinus. No thrombus or stenosis was seen. No collaterals are noted
The upper jugular vein looks normal. One notes in (C) a stenosis in the J2 segment with collaterals bridging the area of stenosis and entering the inominate vein. Generally, this would be considered a hypoplastic segment. However I have started to see that muscular compression can cause this appearance.

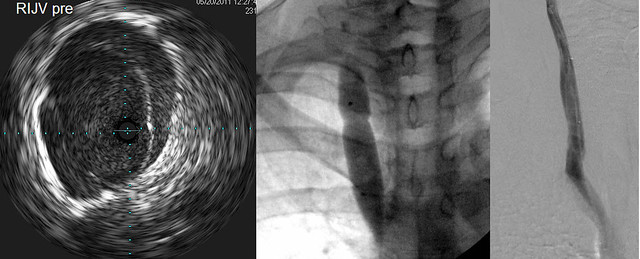
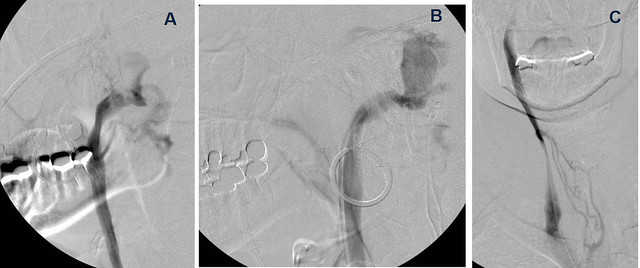
Figure A shows narrowing of the J2 segment. When i asked the patient to turn her head to the left and repeated venography (Figure B), the vein looks normal. the collaterals are not visualized.
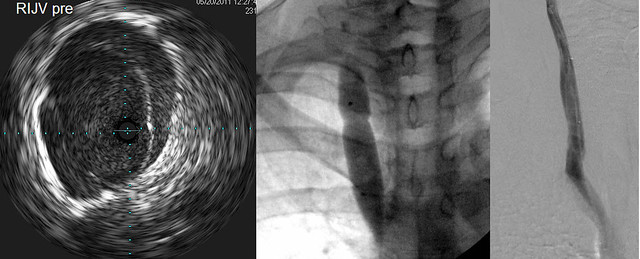
IVUS (left) showed a thickened valve which did not completely open at any time during interrogation.
Angioplasty (center) showed a modest narrowing in the balloon at nominal pressure.
Post procedural angioplasty (right) showed improved flow
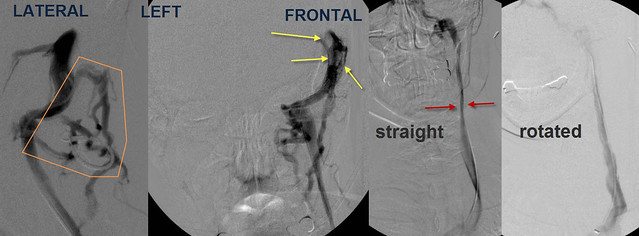
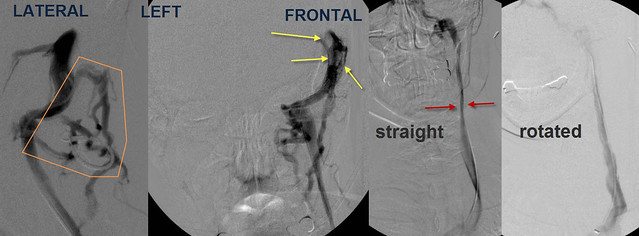
Selective catheterization and venography of the left sigmoid sinus showed that unlike the right side extensive collateral veins were noted in the back of the neck (orange) Also noted were filling defects, consistent with thrombus, in the sinuses. Frontal venogram of the L IJV showed narrowing in J2 (red arrows) similar to the right side. Again, upon rotation of the neck, flow was improved and diameter was normal.

IVUS showed that there was echogenic material in the sigmoid sinus and jugular bulb (orange stars Image A&B). In the upper jugular vein in J3 IVUS showed a thrombus (orange arrows). More distally at the confluens a septum was seen narrowing the jugular lumen (curved orange arrows)

First high pressure angioplasty was performed at the confluens with the subclavian vein. Then the sigmoid sinus was flushed with heparinized saline Then suction was applied to the jugular bulb. Finally, a thrombus was aspirated from the internal jugular vein. This thrombus appeard dark and dense and i believed it was old thrombus. After these three maneuvers, there was brisk flow in the internal jugular vein.

Finally the third major vein was studied. Azygous venography looked very good; no stenoses or webs were seen
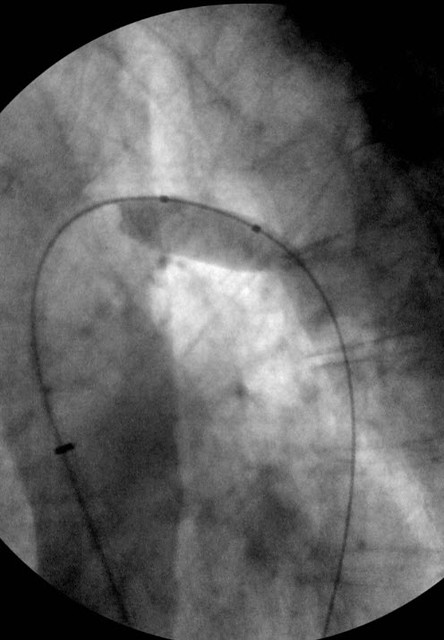
But look at this IVUS of the anterior aspect of the Azygous Arch.

There is a large septum (curved orange arrows) and webs (green arrow) that are compromising the lumen of the vein.
These were treated by balloon angioplasty
pretty interesting case, eh? It's a quite challenging and informative case but this is not the end of it. . As you know, it is recommended that the key collateral networks of the aygous vein be imaged.These include the left renal vein and the ascending lumbar vein. That is why venous entry from the left side is recommended so that these veins can be imaged.
So first i looked at the left renal vein:

The green arrow points to the catheter in the renal vein. There is no contrast in the renal vein. rather the renal vein drains through the hemiazygous vein and outlines all the lumbar veins and the vertebral plexus.
This is a tremendous amount of blood to add to the azygous vein and vertebral plexus. The left renal vein drains about 500 ml of blood/minute. The entire brain drains approximately 750 ml of blood/minute. Thus this venous obstruction almost doubles the blood in the cerebrospinal blood pool, not good when the aygous and its collaterals, and the the internal jugular veins have stenoses!

IVUS of the renal vein shows that there are webs within the renal vein in the kidney itself (yellow arrows). The renal vein draining into the inferior vena cava is pancaked (green arrows)
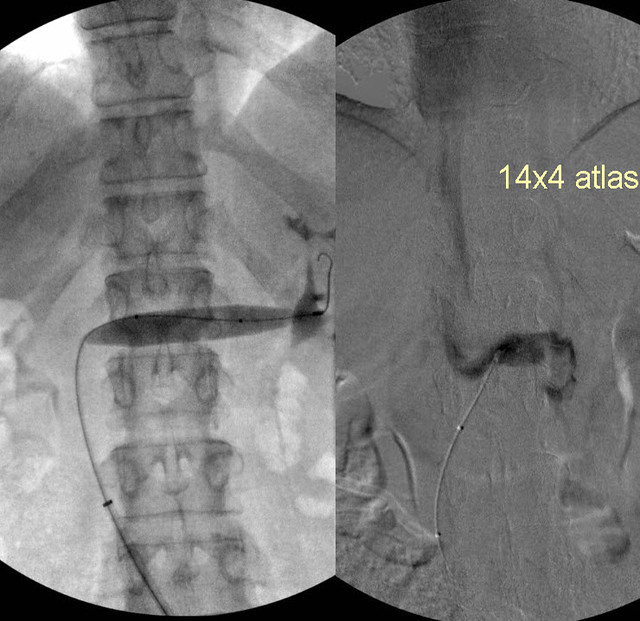
Angioplasty was attempted but this gave only marginal improvements. I am going to bring the patient back for a second treatment of the renal vein, stenting is planned.

Finally inferior vena cavogram (A) and ascending lumber venogram (B) show that the ascending lumbar vein is smaller than the hemiaygous vein (C). Thus renal venous flow is driven by pure dimensions up the azygous vein rather than down into the ascending lumbar vein into the inferior vena cava.
So that is how i spend my time.
Key points
1. IVUS finds things that are unrecognizable by venography
2. the dural sinuses may cause compromised outflow. Whether MRV or venography are superior is unclear to me. At any rate one or the other probably should be part of the investigation of ccsvi
3. This is not likely restenosis but underdilation and elastic recoil because of the time frame
4. The renal vein is an important vessel to study, especially when the aygous is compromised. The renal vein and the ascending lumbar vein form an important collateral drainage pathway when the azygous is stenosed or they can add stress on the cerebrospinal venous circulation when their normal outflow is compromised.
Any questions?