drsclafani wrote:
But the study that you mention was done a long time ago. More than disproving the existence of CCSVI, it proved that considerable experience is necessary to recognize many of the findings of an abnormal venogram. Indeed, when we first started looking at these stenoses, it was thought that the vein wall was stenotic. It took considerable time and the help of the IVUS to show that the stenosis is most commonly caused by an immobile valve rather than stenosis of the wall of the vein.
Based upon a recent case in a young man, it is my sense that composition and function of the valvular tissue evolves with time.I think that i will share that case with you.
Its nature is such that it is common for abnormalities to be subtle and often unrecognizable by venography in young people with MS. With the progression in time the character of the valvular tissue is altered, becoming thicker with age. With aging the vein above the obstruction distends and makes the stenosis more obvious. As the valve thickens, it may become more noticeable. With the vein obstructed, the collateral veins enlarge and the orifice dilates to accomodate the flow. I believe there are obstructions that cannot be identified by the venogram at a young age. Even with IVUS the valvular stenosis and immoblity may be subtle and at some oint be imperceptible.
The case in point illustrates this point. I plan to go back and review the IVUS exams of the youngest patients and compare them to those who have had the disease for a considerable time.
This is a 20 year old Greek man who has had symptoms of multiple sclerosis since age 15. His major problems are difficulty in walking, predominantly because of spasticity caused by upper motor neuron disease. He has weakness in the right foot, with a foot drop, light numbness in the right finger , imbalance, temperature intolerance and fatigue. He had several exacerbations while taking avonex, but becamse exacerbation free while taking natalizumab (tysabri). When tysabri was stopped and copaxone was given he had several exacerbations. While currently taking natalizumab, he has had no exacerbations. He had two doppler exams, i(n Athens by Dr Liasis and in my office in Brooklyn) which showed signs consistent with CCSVI. His neurological examination showed slight nystagmus, absent vibratory sense in both lower legs and feet, an intention tremor and severe spastic weakness in both lower extremities. Rhomberg's test was positive Babinski was positive bilaterally. Clonus of both ankles was present.
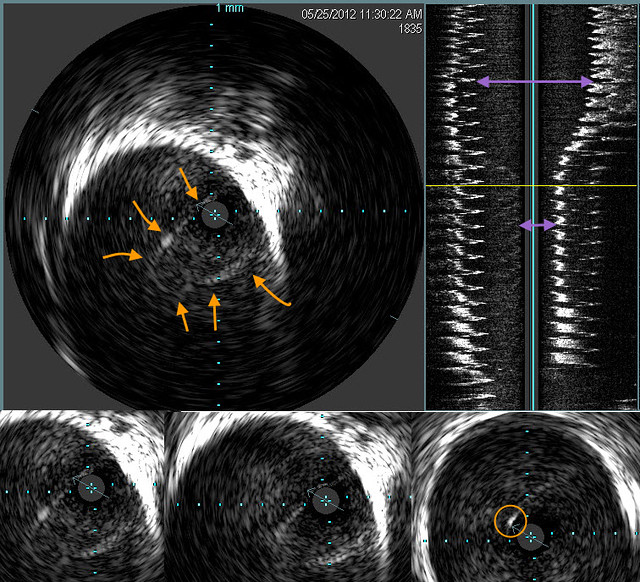
Venography of the right internal jugular vein seemed pretty normal. However there was a subtle finding of possible jet effect (orange arrow).

However the IVUS was quite obvious
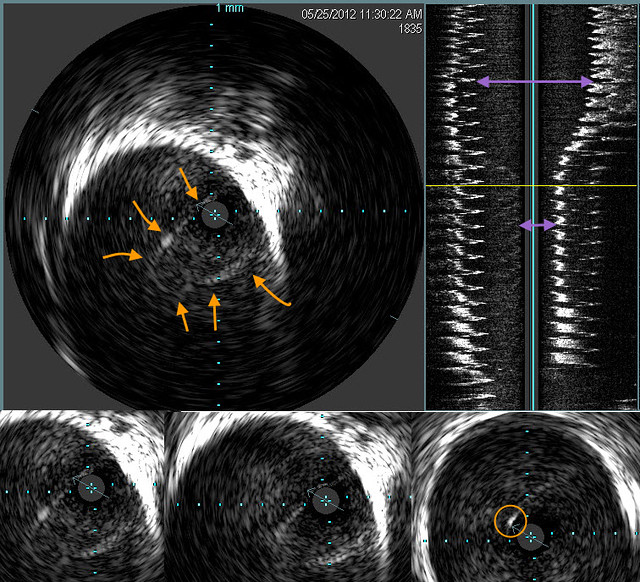
The orange arrows outline an immobile valve that funnels down to a high degree of obstruction.The purple double arrows show how great was the stenosis. However the echogenic area of the vein is not pronounces and the valve was barely visible on IVUS. I have circled in the righ right lower image a thickened focus of echogenic material in the valve .
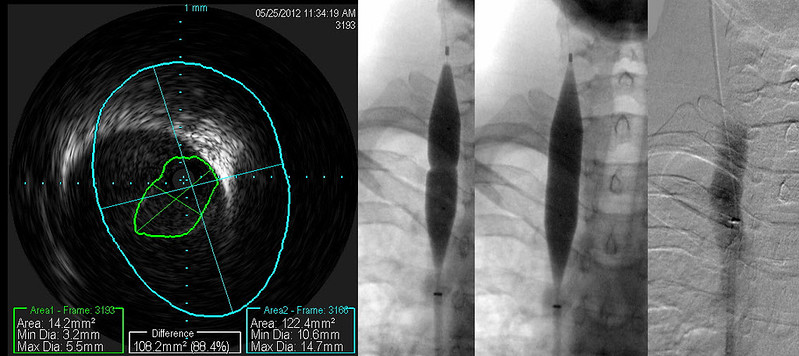
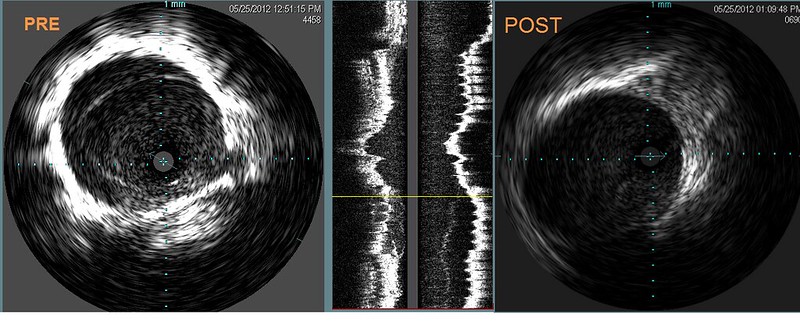
You can see the effective expansion of the vein on this patient's post angioplasty image. A small area of buckled valvular tissue is still within the lumen. Nowever an annular valvular stenosis is no longer present.

The findings were more subtle on the left side. I can discern no clues (except some possible puddling of contrast media within the cusp of a normal appearing venogram). The small amount of opacification of a condylar emissary vein is within normal appearance. It is interesting that the patient has not posterior skull base head and neck ache. I strongly suspect that this headache is due to distension of the posterior cervical veins.

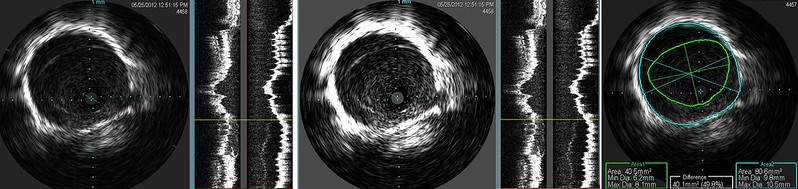
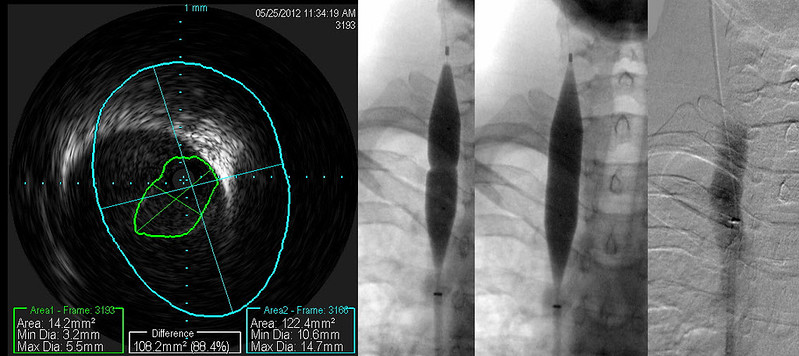
The degree of echogenicity of the valve is not great but sufficient to make it perceptible. I will find a case of long standing CCSVI in a patient with more than 20 years of MS. The difference is striking.
IVUS shows valve pretty clearly. Despite watching this valve orifice for more than one minute, it never opened. Suprisingly, the stenosis measured 67% and nothing was apparent on the venogram.

Venoplasty was performed. I think that the balloon sizing was very good. Although IVUS after venoplasty shows some residual valve tissue in the lumen (arrow), The narrowing ring of tissue has been disrupted and we have not risked injury to the vein. A larger balloon might have given a better picture, but I am not a photographer.

The azygous venogram looks pretty good too, although I would prefer to not see so much reflux. I am concerned by reflux but reflux alone does not tell me where to dilate. I would prefer not to do indiscriminate venooplasty.
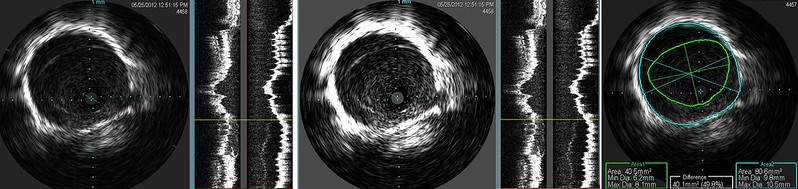
Again IVUS is not equivocal in this case. I showed the same image in two different brightness/contrast levels to illustrate how subtle it can be. Image too dark and it can very difficult to see the immobile valve. Looking at this abnormality, i was not impressed by the degree of stenosis on visual terms. But the IVUS calculation show this to be just about a 50% stenosis. More than the eye can tell.
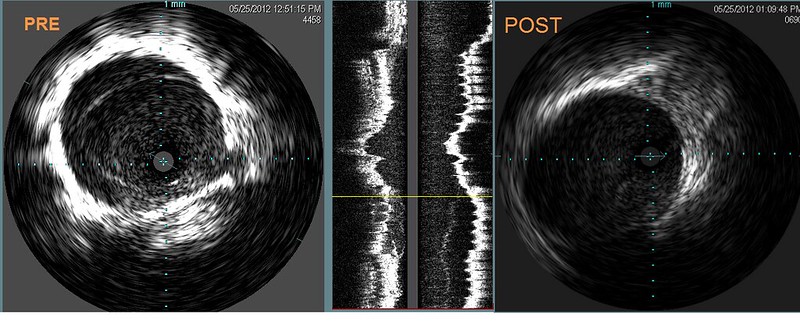
The post venoplasty image shows that no obstruction is present.
Such a case illustrates how even the accepted Gold Standard may miss stenoses in apparently normal looking venograms. Venography is less than perfect because the disease is not generally of the vein itself. But rather of the valve which is much better visualized by IVUS.
I am going to evaluate my speculation that the IVUS appearance changes with duration of disease or with age.
DrS