I think we need to pursue the endovascular approach as much as possible for several reasons.NZer1 wrote:Hi Dr, I have noticed that the vavles when opened are very complex (pathology studies). They appear to be quite a challenge when you look at how they attach and how they are situated to allow for vein enlargement and remain functional, almost a spiral where they attach.
Is it possible that these are going to in 'some' cases require removal as opposed to stretch to overcome their blocking effect. My thought is that at some point there will be indications which are best treated in curtain ways.
If the problem types were identified and some how their position recorded is it possible that some form of micro surgery could access and remove the dysfunctional value completely? In my mind it seems that some of these problem puppies may need to be removed rather than be an on going, on growing issue hanging in there. Not very technical explanation, but simple is good
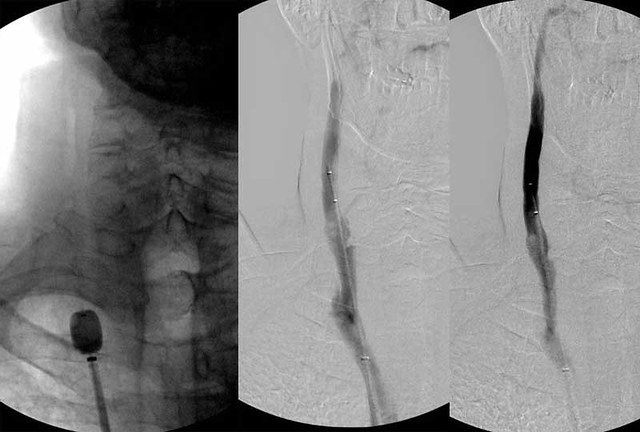
1. Veins are tempermental. They can get down right petulant when disturbed. Especially when flow is slow. Of course, I am not a carpenter, just a plumber, but you must understand that the valves are in a challenging area, just below the clavicle. As such surgery can be quite challenging there.
2. Less invasive is good: it reduces the logic for resistance to treatment
3. Rapid throughput is essential: for the moment, it would take years to treat everyone (not saying that everyone needs treatment yet) given the limited numbers of operators.
lets figure out when the endovascular approach is not effective, then work out alternate therapies.

 [/quote]
[/quote]