AlmostClever: Can I assume that doppler and Bmode ultrasound was performed before the procedure? And why are you having a second procedure? did you have worsening of symptoms?AlmostClever wrote:Dr. Sclafani,
I had a venogram today which revealed my right IJV is completely occluded.
This vein was open a month ago, but the treating doctor could not get the wire through this time.
Any suggestions on how to treat a completely occluded vein like this one that was open a month ago?
Thanks for your help!
AlmostClever
At any rate, ultrasound is very important when one cannnot get the guidewire to pass an obstruction. The differential diagnosis includes
1. complete thrombosis with hard thrombus,
2. high grade stenosis that prevents the entry of a wire or catheter
3. the catheter has gone into an incomplete duplication
4. not enough persistence.
Ultrasound is very important because we must diagnosis #1 or exclude it.
If the vein above the occlusion is not thrombosed, there will be sonolucency and compressibility of the jugular vein on ultrasound.In such circumstances the interventionalist can continue to try or failing a reasonable persistent attempt, one can attempt a rendevous procedure.
Allow me to demonstrate a rendevous procedure.This is about a forty year old woman with fatigue, weakness, temperature intolerance, the usual general symptoms
Doppler and B mode ultrasound of the neck and power doppler examination of the deep cerebral veins by ccsvi technique showed three positive signs.
Therefore venography was performed.
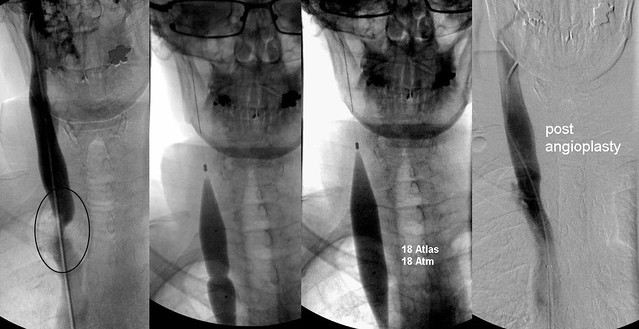
Examination of the right neck showed a single annular stenosis. This was treated by high pressure large balloons with wide expansion of the vein and good flow.
subsequently cathterization of the left jugular vein was attempted. This proved impossible despite probing with several different catheter shapes and three different guidewires for almost one hour.
A rendevous procedure was then attempted. the left neck was prepped to sterility. A Bmode ultrasound readily visualized a small but pateent jugular vein in the region of J2. Using ultrasound guidance and micropuncture technique, the vein was accessed and a platinum tip guidewire was advanced easily into the central part of the IJ vein.
In a true rendovous procedure, one would grab the guidewire in the chest with a snare entering the neck puncture and pull the guidewire up into the higher jugular vein. Then the procedure could continue.
in this case we were able to track along the US placed neck guidewire and ultimately get a catheter up the neck.

Figure A shows the catheter unable to advance. Contrast media ends blindly and does not go up into the upper jugular vein.
Figure B is after a rendevous manuever. The catheter is now in the upper jugular vein. Contrast media does not travel towards the chest (red arrow) because the 1.66 mm catheter blocks all flow. The orange curved arrow shows flow up into the dural sinus and finally down the recently fixed right jugular vein (white arrow)
Figure C shows that some drainage occurs down the enck via the vertebral veins (green arrow)
Figure D shows an anterior jugular collateral.
So a hypoplasia correction procedure was performed in one treatment.
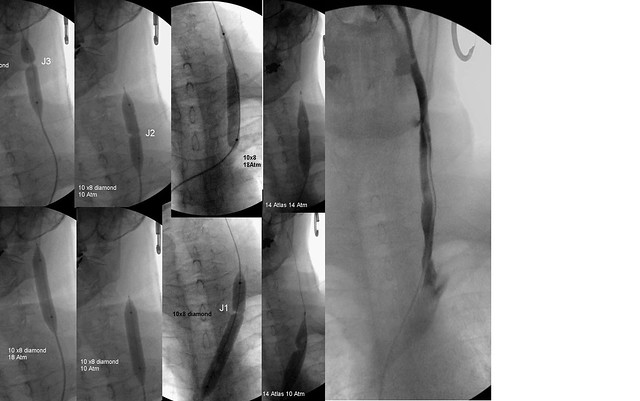
First 10 millimeter 8 cm long balloons were used to dilate the J3, J2 and J1 regions. 10 Atmospheres were sufficient to overcome all stenoses except annular stenosis at the confluens. Finally 14 mm balloons were used to overcome stenotic areas in J1.
the final image on the right shows the ultimate appearance of the veins. No collaterals were noted..
one would anticipate that this patient has notseen her last day in this department.
not a bad beginning but reconstruction may take more than one treatment. So we come to another question, should periodic dilatation be performed or is one treatment sufficient until restenosis. This is unanswered. at the momen


