Cece wrote:drsclafani wrote:Recently, i decided to begin my interrogation of the jugular veins by evaluating the juction between the sigmoid sinus and the jugular bulb and the jugular vein.
Does it change any of your choices during the procedure, if an issue is found there?
yes. i am in the process of writing about an experience this past weekend. Thought i had it finished last night but a glich pushed it back to today.
detecting something at the junction of jugular vein, jugular bulb and sigmoid sinus is important.
I think you just must see the entire vein.
So here it is:
I have learned many things in the past few months.
Among changes in my techniques are:
1. Venous access through the left saphenous vein using ultrasound guidance.
2. Begin the treatment by sigmoid sinus venography
3. Intravascular ultrasound
4. high pressure balloon angioplasty to a size between 50-100% above the nominal cross sectional area of the measured vein.
5. Avoidance of the use of stents except under the following theoretical circumstances:
a. restenosis after angioplasty
b. resistant stenosis
c. occlusion not responding to angioplasty
d. in-stent stenosis
e. unfavorable intimal flap or dissection
This weekend I treated a 41 year old Swiss woman with SPMS that tested a couple of these concepts.
Her initial symptoms in 1996 were optic neuritis and she went on to develop left lower extremity, left upper extremity and truncal weakness associated with spasticity. She lacks balance, has severe fatigue and heat intolerance, and suffers from migraine-like headaches. She has urinary urgency and constipation. After 10 years of copaxone, she currently is on no disease modifying medications.
In March 2010 she underwent her first CCSVI treatment in an eastern European country. At that time, stenosis of the lower right internal jugular vein was treated by a 10 mm angioplasty followed by 12 mm stenting. She received no benefit from this procedure.
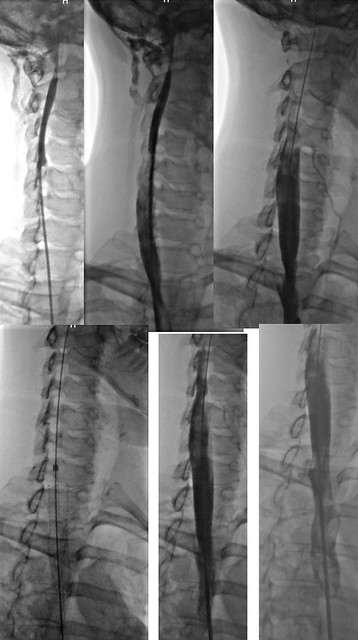
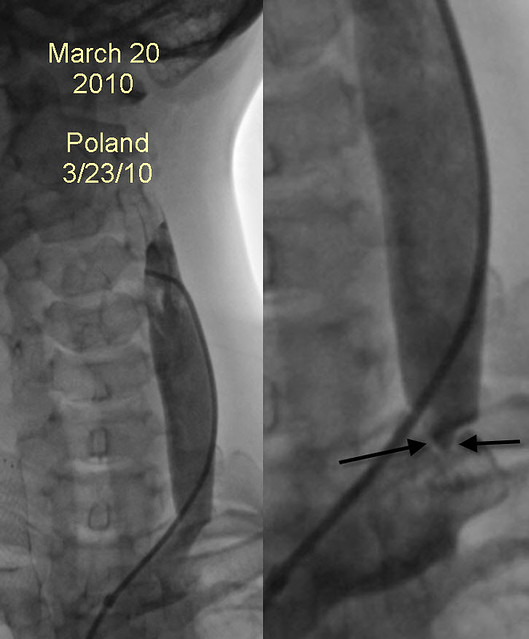
right IJVenography showed a 50% stenosis of the right IJV at confluens with residual stenosis after 10 mm angioplasty. Thus a stent was place (12mm by 4cm) in the J1 segment. The stent was low and covered the origin of the right subclavian vein.
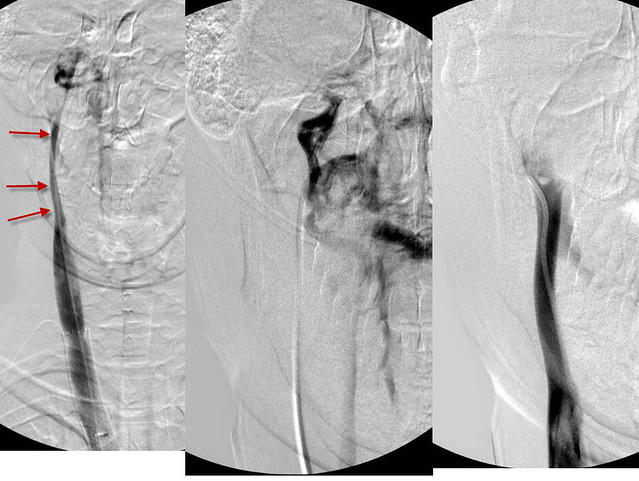
Note that the upper J3 segment of the vein appears assymetrically narrower than the remainder of the jugular vein. No treatment was offered.
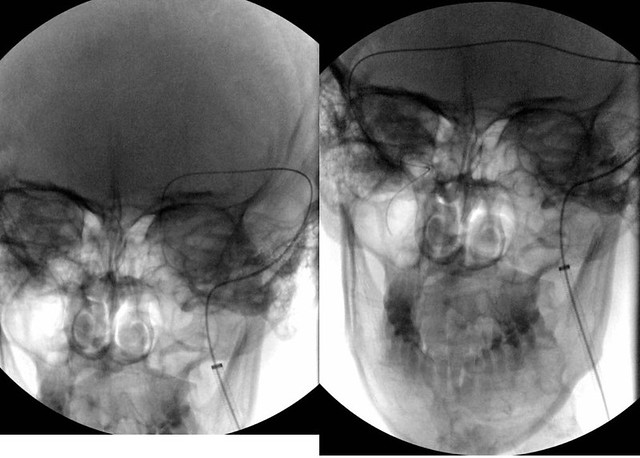
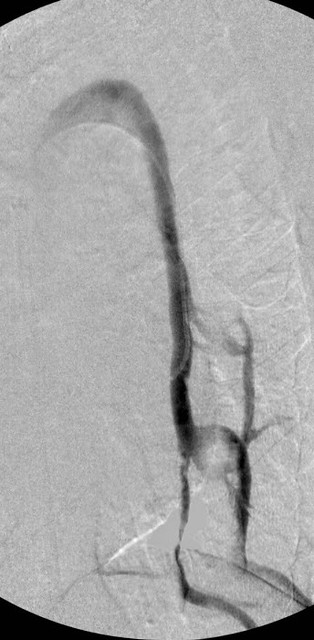
The image on the left looks unremarkable but on closer review of other images in the sequence (IMAGE ON RIGHT), a jet, suspicious for a high grade stenosis of the confluens is seen. Unfortunately, it was not recognized at that time and no angioplasty was performed. Moreover the left upper jugular vein was not visualized.
In November 2010 she had her procedure repeated in Alexandria .

The examination in Egypt showed some intimal hyperplasia of the junction of the stent and the nonstented vein above the stent. The upper IJV was not imaged. After angioplasty, the mild intimal hyperplastic narrowing was no longer seen. No additional stenting was performed.

The high grade stenosis underestimated in march 2010 was again seen. Her left internal jugular vein was treated by 12 mm angioplasty with a cutting wire ("poor man's cutting balloon"). It appears that this angioplasty was considered satisfactory.

However venography clearly shows persistent stenosis (ARROWS).
Angioplasty of the azygous vein was also performed.
She received limited and short term relief.
It is not my intention to show others' errors. We ALL made mistakes and misinterpretations and probably continue to do so as this is a different presentation that we all assumed at the beginning. I remember thinking that this was simple, and looking at dr Zamboni's papers i felt justified in thinking this. But with time, the subtle nature of some of the abnormal imaging presentations have become clearer.
So having set the table, I share with you my experience.
As you know, I still find it difficult to complete three cases in a day, but feel compelled to treat as many patients as possible, safely and accurately. So it was with some satisfaction that i had completed my second procedure on Friday by 1pm with the aim of leaving the center by the decent time of 5pm. Would that it were true!
I initially catheterized the right internal jugular vein.
there is mild intimal hyperplasia at the top of the stent resulting in minor stenosis. However note that the upper reaches of the right IJV are not visualized. Attempts to advance a guidewire only resulted in mild contrast extravasation. There was very good flow but it was unclear whether this was from collateral vessels entering the IJV or from direct flow from the head.
i left the right jugular with an intention to return there depending upon what i found in the other vessels.
Left IJV venography was next performed.
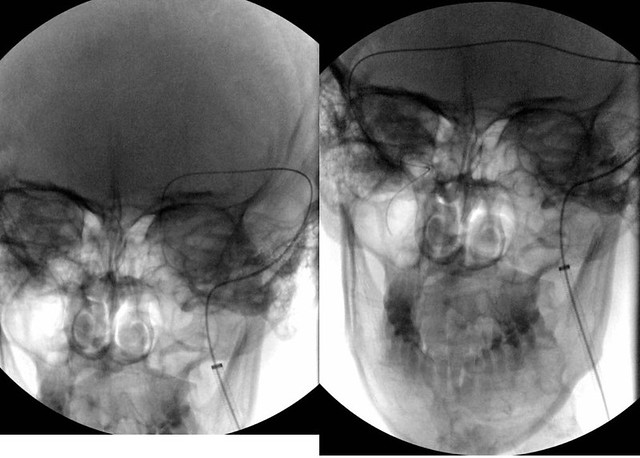
Initially the guidewire was advanced through the left jugular bulb into the sigmoid sinus. Then it was advanced across the transverse sinus, into the right sigmoid sinus and finally past the right jugular bulb and into the the jugular vein.
I finally knew the location of the highest part of the right internal jugular vein and that there was a lumen of the vein.
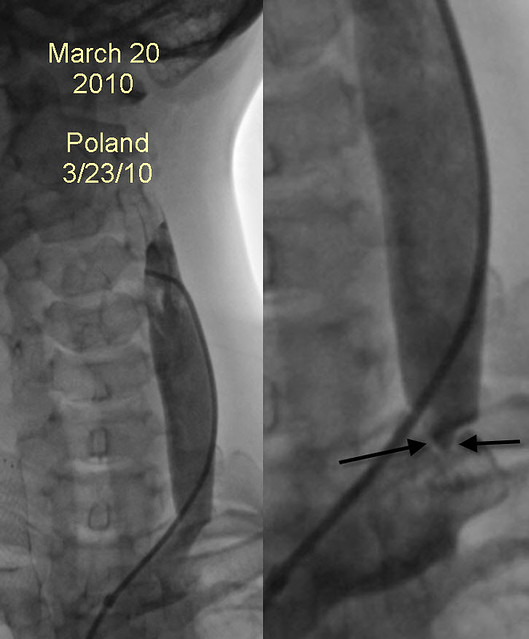
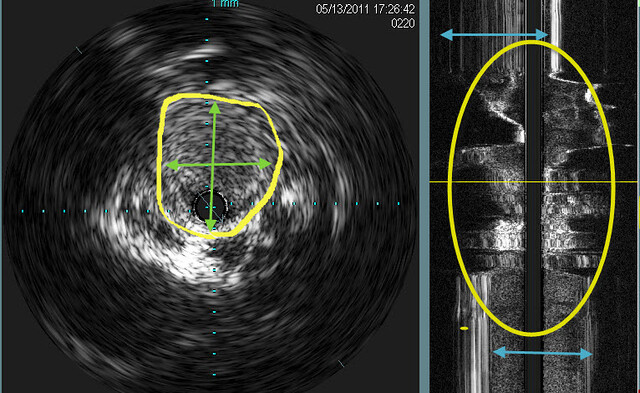
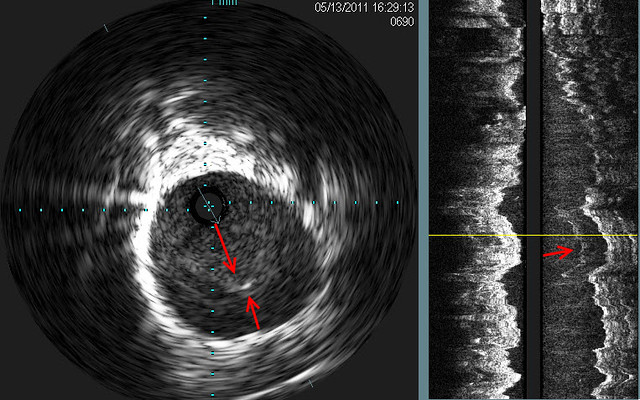
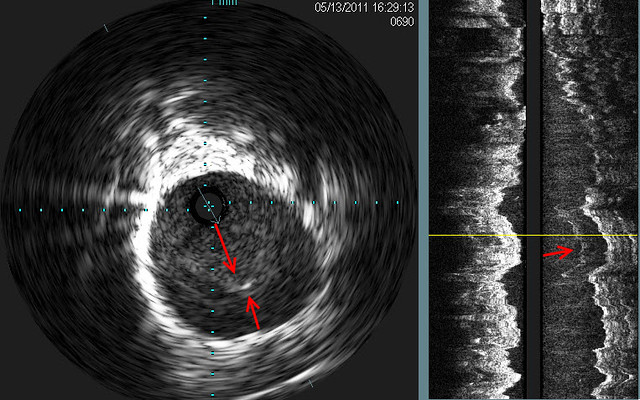
before returning to the RIJV, left IJV venography was performed. It showed a subtle "jet" of contrast media (red arrows). Intravascular ultrasound showed a septum across the ostium of the left IJV at its entrance into the left subclavian vein. on the sagittal view, the septum was represented as scattered white lines (red arrow) on IVUS
Venoplasty clearly shows the "waist" on the balloon and after 14 atmosphered of pressure were applied, the "waist was no longer seen. I wonder whether this will also represent a challenge as Nunzio's left jugular was!

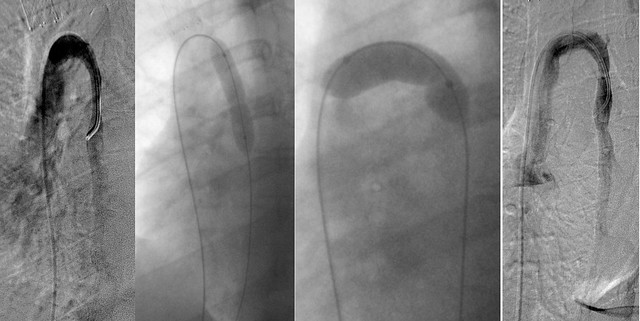
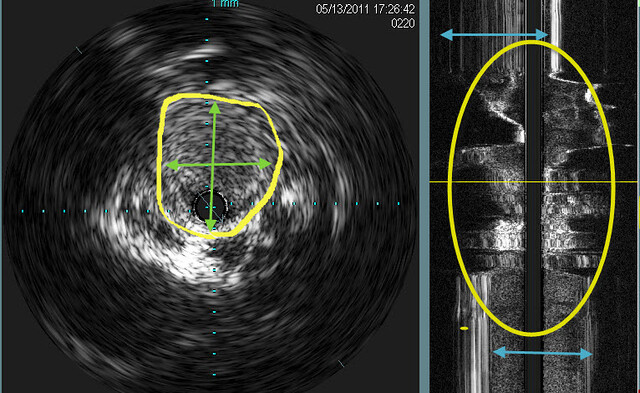
Now i returned to the right IJV. repeated attempts to advance the guidewire were performed for several minutes with no success. Then the guidewire advanced with a push up and into the jugular bulb and canal. Eventually the wire was placed within the right sigmoid sinus and IVUS was done.
Ivus showed that there was occlusion of the upper segment of the RIJV.
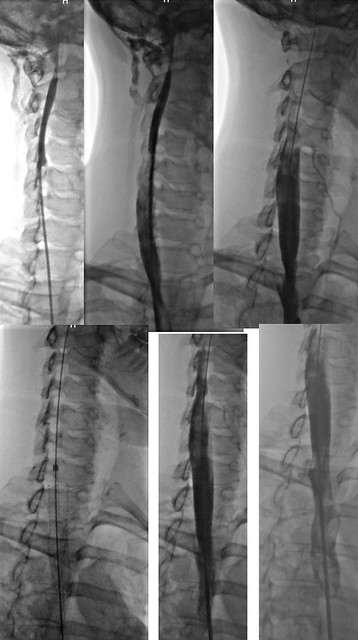
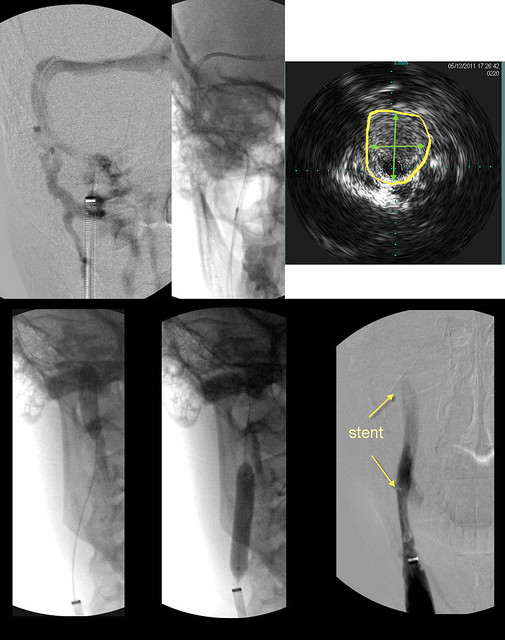
The next image is a composite that summarizes the intervention done on the J3 segment of the RIJV
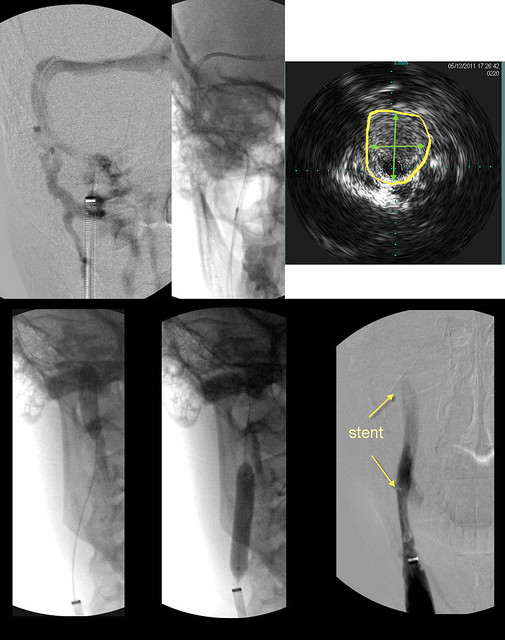
UPPER LEFT image shows contrast in the sigmoid sinus. However the upper jugular vein was not seen. Collaterals in the neck and spine were seen.
UPPER MID: A second wire was advanced as a safety wire and over it was placed an IVUS probe. (dark spot)
UPPER RIGHT: IVUS shows an occlusion of the upper jugular vein. Measurment of diameters of occlusions is not easy by venography, but IVUS is quite precise (YELLOW ARROWS).
LOWER LEFT & MIDDLE: 8mm by 6cm angioplasty performed. However there was no flow on angiography.
LOWER RIGHT: Therefore a stent was placed8mm by 4cm. Venography shows flow.
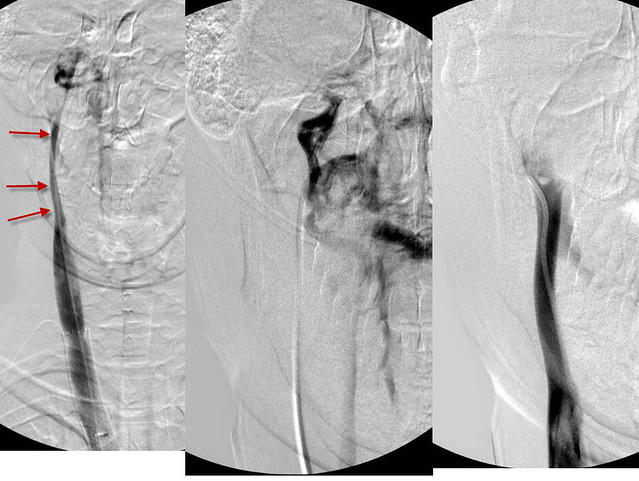
Finally, we imaged the azygous vein.
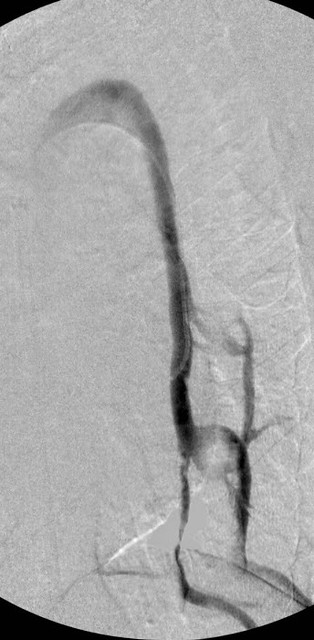
the image looked pretty good to me. However there was a persistent immobile valve that was treated by balloon angioplasty.
Finally in the ascending azygous vein i noted some funky looking echoes. These likely represent webs.
So that the story of my patient and me on a late Friday night date.
hopefully she will receive some benefits of this.
Things i learned are that
1. prior treatments may not be durable
2. Early treatments overlook things
3. the entire jugular vein must be imaged
4. there is a role for stents
5. webs may be visible on IVUS
any questions?




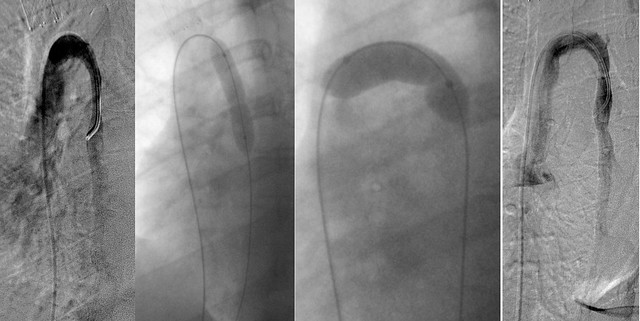

 Finally in the ascending azygous vein i noted some funky looking echoes. These likely represent webs.
Finally in the ascending azygous vein i noted some funky looking echoes. These likely represent webs.