i think that this was old clot. i didnt think that it would respond to thrombolytic agents. a mechanical thrombectomy device might have been helpful but i did not think it would go through the jugular bulb and canal. So the best i could do was flush the clots, hopefully down the other sigmoid sinus which was already opened and the jugular had great flow on that side. some of the clot came down the left and some of that got hung up in J3. A large bore open mouthed catheter was used to suck out the clot. the tissue was very hard and firm suggesting that it was an old clot. Perhaps it was a residual of the prior ccsvi procedureCece wrote:Will there be any treatment for the patient's sinus thrombosis?drsclafani wrote:
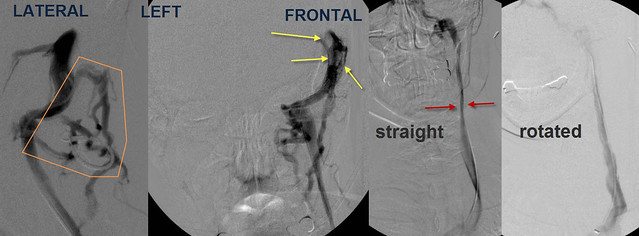
Selective catheterization and venography of the left sigmoid sinus showed that unlike the right side extensive collateral veins were noted in the back of the neck (orange) Also noted were filling defects, consistent with thrombus, in the sinuses. Frontal venogram of the L IJV showed narrowing in J2 (red arrows) similar to the right side. Again, upon rotation of the neck, flow was improved and diameter was normal.
this was an incomplete thrombus. such things can cause symptoms simular to ccsvi. (well known)Did the patient have any symptoms of sinus thrombosis or a guess as to when it occurred in the patient history?
no normal looking neck. at this time i am not convinced about ctos. i want to treat first and see if there is improvement.Was there any external/physical appearance to the neck to suggest the problematic muscles? Was CTOS discussed? Could neck stretches help these muscles loosen up?
So we will treat the renal vein first.