all things vitamin D
- notasperfectasyou
- Family Elder
- Posts: 802
- Joined: Thu Feb 09, 2006 3:00 pm
- Location: Northern Virginia
- Contact:
Kim is taking D3 8000-9000/day. She got a script from her Neurologist for 50000 once a week, but our farm'acy only had D2 and we wanted D3. So he said it was ok to continue on the ones we get OTC. But, Kim has been on high dose D from even before that. There is a lot of stuff out there on it. Ken
It would be really nice to be able to put links in here
If I have included a bad link, google the word "Scholar", click link for "Google Scholar". Search for the name of the paper and author in Google Scholar.
If I have included a bad link, google the word "Scholar", click link for "Google Scholar". Search for the name of the paper and author in Google Scholar.
My husband only tests his D levels once or twice a year when he goes in to see one of his doctors. He takes 5000 IU/day, and he's usually at around 50ng/ml. That's about 125nanomoles/liter, I think. We're going to try to creep him up a little higher though.
--Mamacita
http://multiplesclerosisrecipes.blogspot.com/
--Mamacita
http://multiplesclerosisrecipes.blogspot.com/
- notasperfectasyou
- Family Elder
- Posts: 802
- Joined: Thu Feb 09, 2006 3:00 pm
- Location: Northern Virginia
- Contact:
I don't know if the bumps Kim's had on her face is Eczema, but when she started on ABX, it cleared up. Ken
It would be really nice to be able to put links in here
If I have included a bad link, google the word "Scholar", click link for "Google Scholar". Search for the name of the paper and author in Google Scholar.
If I have included a bad link, google the word "Scholar", click link for "Google Scholar". Search for the name of the paper and author in Google Scholar.
-
Wonderfulworld
- Family Elder
- Posts: 776
- Joined: Sun Aug 27, 2006 2:00 pm
- Location: Ireland
- Contact:
I am on 4000IU D3 a day.
Two things happened about 5 months after starting the regime.
I stopped having monthly migraines.
My dishydriotic eczema cleared up.
I recently had a flare up but it was mainly sensory symptoms and brain fog and seems to be clearing up without the "take to the bed for a month" routine that it normally takes, this time of year.
I have a good feeling about it too.
Two things happened about 5 months after starting the regime.
I stopped having monthly migraines.
My dishydriotic eczema cleared up.
I recently had a flare up but it was mainly sensory symptoms and brain fog and seems to be clearing up without the "take to the bed for a month" routine that it normally takes, this time of year.
I have a good feeling about it too.
~~~~~~~~~~~~~~~
Concussus Resurgo
~~~~~~~~~~~~~~~
RR-MS dx 1998 and Coeliac dx 2003
~~~~~~~~~~~~~~~
Tecfidera, Cymbalta, Baclofen.
EPO, Fish Oils, Vitamin D3 2000 IU, Magnesium, Multivitamin/mineral, Co-Enzyme Q10, Probiotics, Milk Thistle, Melatonin.
Concussus Resurgo
~~~~~~~~~~~~~~~
RR-MS dx 1998 and Coeliac dx 2003
~~~~~~~~~~~~~~~
Tecfidera, Cymbalta, Baclofen.
EPO, Fish Oils, Vitamin D3 2000 IU, Magnesium, Multivitamin/mineral, Co-Enzyme Q10, Probiotics, Milk Thistle, Melatonin.
ww i'm going to relay that info about d3 helping your migraines, to a friend.
i went looking for other things that happen in the skin besides making d3, when exposed to sunlight. because my d3 status is great but my skin still sucks. so yesterday i learned about fumaric acid. i wonder what the heck else the skin makes when exposed to UV???
anyway, so now i'm sort of wrapped up in fumaric acid, and serum levels of that other metabolite of d3 1,25 dihydroxycholecalciferol, and phosphate and child levels vs adult, renal function, etc etc...
i will let you know if i figure out how to cure my skin too lol
in the meantime, still keeping tabs on the d3. was at the lab yesterday, gave some blood to see if i'm back down in the 100-250 range again, after a month and a half off from d3 supplements (still eating fish though).
ttfn,
JL
i went looking for other things that happen in the skin besides making d3, when exposed to sunlight. because my d3 status is great but my skin still sucks. so yesterday i learned about fumaric acid. i wonder what the heck else the skin makes when exposed to UV???
anyway, so now i'm sort of wrapped up in fumaric acid, and serum levels of that other metabolite of d3 1,25 dihydroxycholecalciferol, and phosphate and child levels vs adult, renal function, etc etc...
i will let you know if i figure out how to cure my skin too lol
in the meantime, still keeping tabs on the d3. was at the lab yesterday, gave some blood to see if i'm back down in the 100-250 range again, after a month and a half off from d3 supplements (still eating fish though).
ttfn,
JL
JL,jimmylegs wrote:i went looking for other things that happen in the skin besides making d3, when exposed to sunlight. because my d3 status is great but my skin still sucks. so yesterday i learned about fumaric acid. i wonder what the heck else the skin makes when exposed to UV???
anyway, so now i'm sort of wrapped up in fumaric acid, and serum levels of that other metabolite of d3 1,25 dihydroxycholecalciferol, and phosphate and child levels vs adult, renal function, etc etc...
i will let you know if i figure out how to cure my skin too lol
JL
This is interesting you mention fumaric acid. One of the drugs in phase III trials right now, BG12, is dimethyl fumarate, an oral fumarate derivative. And another interesting thing, since you mention your skin, is that it was originally developed (or at least used) as a treatment for psoriasis.
Why Low Vitamin D Raises Heart Disease Risks In Diabetics
Treatment: Gilenya since 01/2011, CCSVI both IJV ballooned 09/2010, Tysabri stopped after 24 Infusions and positive JCV antibody test, after LDN, ABX Wheldon Regime for 1 year.
Vitamin D and the higher incidence of AI diseases in Women
http://www.examiner.com/x-16026-Napa-Co ... s-in-women
Vitamin D and the higher incidence of autoimmune diseases in women
It has long been observed that autoimmune diseases like lupus and multiple sclerosis are more common in women than in men. Other related chronic conditions such as osteoporosis, osteoarthritis and chronic fatigue syndrome are also much more common in women as well. Two research papers published in the upcoming September, 2009 special issue of the Annals of the New York Academy of Sciences, titled Contemporary Challenges in Autoimmunity, show a possible connection that involves vitamin D and how it is metabolized in the body.
Vitamin D (also called cholecalciferol) is important in both men and women, and at first glance it would seem that it should behave the same way in both sexes. It has no role in sex-specific hormonal regulation like some of the sex hormones, but it has recently been discovered that a special molecule, called a receptor, that binds to one of the forms of vitamin D is more abundant in women than men. The receptor to which vitamin D binds is important in the activation of the innate immune response.
The vitamin D receptor (VDR) is found in the nucleus of certain cells throughout the body. Recently it was discovered that women have more of these receptors, because in addition to all the same kinds of cells shared with men, they also have VDRs in endometrial cells. Endometrial cells, which comprise the lining of the uterus, are cyclical. Therefore, the number of VDRs fluctuates in sync with the menstrual cycle.
The key
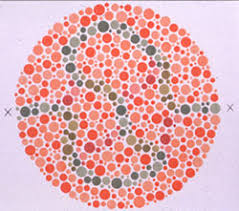
1,25-D, also called calcitriol. This is the form of vitamin D that binds to vitamin D receptors (VDRs). Source: Wikipedia.
to how vitamin D plays its part is to understand what the VDR does. When the correct form of vitamin D (a form known as 1,25-D or calcitriol) binds to VDR, VDR then directly causes the expression of over 900 genes to occur. Two of the genes that are turned on produce proteins that are directly responsible for kicking the immune response into active mode. The reason for VDR in the endometrium is that it provides protection against infection for the developing fetus.
Another key to the puzzle has been the growing evidence that bacteria may play a role in the development of autoimmune disease. If so, why wouldn’t women, who have more VDRs, be better off than men? The problem is that bacteria of various kinds can interfere with VDRs and prevent vitamin D from binding. If vitamin is unable to bind, then the immune response is disrupted. Not only is the immune system affected, but thyroid hormone problems can result too.
Although these results do not provide a clear path to treatment, “the potential role of persistent pathogens in autoimmune disease mandates reconsideration of the use of corticosteroids as a first-line treatment for many autoimmune diseases. Corticosteroids effectively reduce the ability of the immune system to respond to pathogens, including persistent microbiota, which is counterproductive to recovery.”
As a result of the dysregulation of VDRs blood levels of the 1,25-D form of vitamin D increase, because less 1,25-D is binding. “Given the potential benefits of serum 1,25-D as a clinical marker both in the diagnosis and monitoring of treatment response, further research is warranted. If elevated levels of 1,25-D continue to be associated with an inflammatory disease state, 1,25-D could be used as a reliable marker of the autoimmune disease process.”
Sources:
Amy D. Proal, Paul J. Albert, and Trevor G. Marshall. 2009. Dysregulation of the Vitamin D Nuclear Receptor May Contribute to the Higher Prevalence of Some Autoimmune Diseases in Women, In Contemporary Challenges in Autoimmunity. Annals of the New York Academy of Sciences 1173: 252–259.
Greg P. Blaney, Paul J. Albert, and Amy D. Proal. 2009. Vitamin D Metabolites as Clinical Markers in Autoimmune and Chronic Disease, In Contemporary Challenges in Autoimmunity. Annals of the New York Academy of Sciences 1173: 384–390
Vitamin D and the higher incidence of autoimmune diseases in women
It has long been observed that autoimmune diseases like lupus and multiple sclerosis are more common in women than in men. Other related chronic conditions such as osteoporosis, osteoarthritis and chronic fatigue syndrome are also much more common in women as well. Two research papers published in the upcoming September, 2009 special issue of the Annals of the New York Academy of Sciences, titled Contemporary Challenges in Autoimmunity, show a possible connection that involves vitamin D and how it is metabolized in the body.
Vitamin D (also called cholecalciferol) is important in both men and women, and at first glance it would seem that it should behave the same way in both sexes. It has no role in sex-specific hormonal regulation like some of the sex hormones, but it has recently been discovered that a special molecule, called a receptor, that binds to one of the forms of vitamin D is more abundant in women than men. The receptor to which vitamin D binds is important in the activation of the innate immune response.
The vitamin D receptor (VDR) is found in the nucleus of certain cells throughout the body. Recently it was discovered that women have more of these receptors, because in addition to all the same kinds of cells shared with men, they also have VDRs in endometrial cells. Endometrial cells, which comprise the lining of the uterus, are cyclical. Therefore, the number of VDRs fluctuates in sync with the menstrual cycle.
The key
1,25-D, also called calcitriol. This is the form of vitamin D that binds to vitamin D receptors (VDRs). Source: Wikipedia.
to how vitamin D plays its part is to understand what the VDR does. When the correct form of vitamin D (a form known as 1,25-D or calcitriol) binds to VDR, VDR then directly causes the expression of over 900 genes to occur. Two of the genes that are turned on produce proteins that are directly responsible for kicking the immune response into active mode. The reason for VDR in the endometrium is that it provides protection against infection for the developing fetus.
Another key to the puzzle has been the growing evidence that bacteria may play a role in the development of autoimmune disease. If so, why wouldn’t women, who have more VDRs, be better off than men? The problem is that bacteria of various kinds can interfere with VDRs and prevent vitamin D from binding. If vitamin is unable to bind, then the immune response is disrupted. Not only is the immune system affected, but thyroid hormone problems can result too.
Although these results do not provide a clear path to treatment, “the potential role of persistent pathogens in autoimmune disease mandates reconsideration of the use of corticosteroids as a first-line treatment for many autoimmune diseases. Corticosteroids effectively reduce the ability of the immune system to respond to pathogens, including persistent microbiota, which is counterproductive to recovery.”
As a result of the dysregulation of VDRs blood levels of the 1,25-D form of vitamin D increase, because less 1,25-D is binding. “Given the potential benefits of serum 1,25-D as a clinical marker both in the diagnosis and monitoring of treatment response, further research is warranted. If elevated levels of 1,25-D continue to be associated with an inflammatory disease state, 1,25-D could be used as a reliable marker of the autoimmune disease process.”
Sources:
Amy D. Proal, Paul J. Albert, and Trevor G. Marshall. 2009. Dysregulation of the Vitamin D Nuclear Receptor May Contribute to the Higher Prevalence of Some Autoimmune Diseases in Women, In Contemporary Challenges in Autoimmunity. Annals of the New York Academy of Sciences 1173: 252–259.
Greg P. Blaney, Paul J. Albert, and Amy D. Proal. 2009. Vitamin D Metabolites as Clinical Markers in Autoimmune and Chronic Disease, In Contemporary Challenges in Autoimmunity. Annals of the New York Academy of Sciences 1173: 384–390
Vitamin D Pill question
I stopped at GNC the other night to pick up some more Vitamin D pills. They had a brand that are 5000 IU's in a gelcap. Does anyone know if these are for real? They are tiny compared to 1000 IU horse pills I bought last time.