Ann Neurol. 2025 Aug;98(2):294-307.
Objective: To compare clinical and radiological outcomes among relapsing multiple sclerosis patients treated with autologous hematopoietic stem cell transplantation (AHSCT), alemtuzumab (ATZ), and ocrelizumab (OCR).
Methods: From a London (UK) hospital-based observational cohort, modeled data were obtained from 621 relapsing-remitting multiple sclerosis patients, who were treated with AHSCT (n = 103), ATZ (n = 204), and OCR (n = 314), and were followed up for 43, 43, and 32 median months, respectively. The annualized relapse rate, new magnetic resonance imaging (MRI) lesions, and disability progression on Expanded Disability Status Scale were assessed.
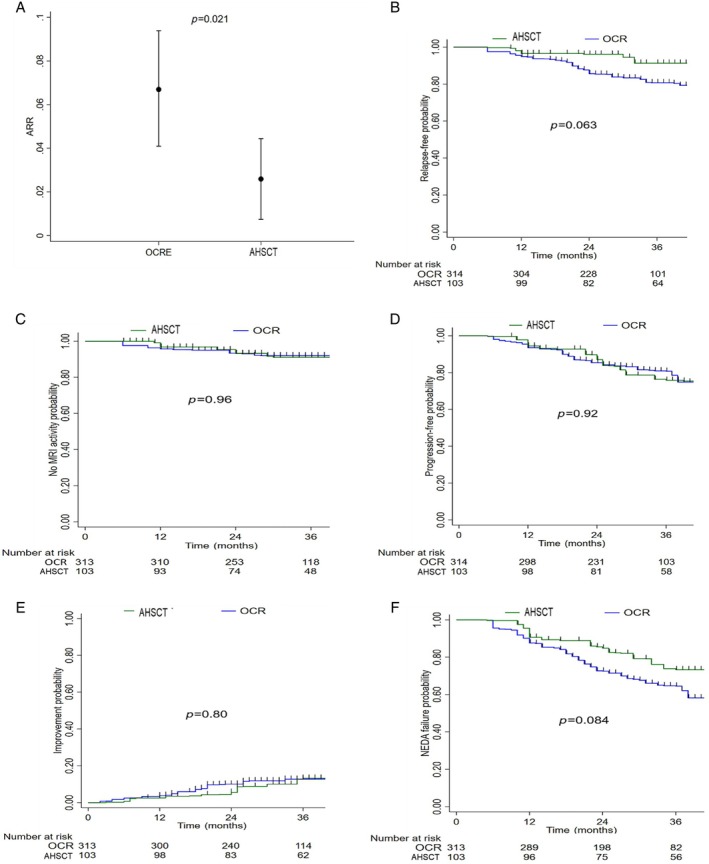
Results: AHSCT showed superior efficacy compared with ATZ and OCR. After 5-year follow up, the mean annualized relapse rate (0.026 vs 0.087; p < 0.001), the risk of relapses (HR 0.29, 95% CI 0.13-0.63; p = 0.002), and of MRI activity (HR 0.33, 95% CI 0.15-0.72; p = 0.006) were significantly lower in AHSCT versus ATZ group. Compared with OCR, after 3-year follow-up AHSCT showed a significantly lower annualized relapse rate (0.028 vs 0.073; p = 0.02) and a trend to reduced risk of relapse (HR 0.45, 95% CI 0.18-1.14; p = 0.09), but similar low rates (6%) of new MRI activity (HR 0.86, 95% CI 0.28-2.67; p = 0.80). In addition, there was a similar risk of Expanded Disability Status Scale progression in AHSCT, and both ATZ (HR 1.19, 95% CI 0.71-2.00; p = 0.50) and OCR (HR 1.08, 95% CI 0.57-2.04; p = 0.82) groups.
Interpretation: AHSCT was followed by greater prevention of relapses compared with ATZ and OCR, and suppressed more profoundly MRI activity than ATZ, but similarly to OCR, albeit with shorter follow up. The risk of accumulating disability was similar among the treated groups. Studies with larger sample sizes and longer follow up may enable confirmation of these findings or detection of any additional differential effects.
[Free full text]
Figure 2: Stem cells vs. Campath
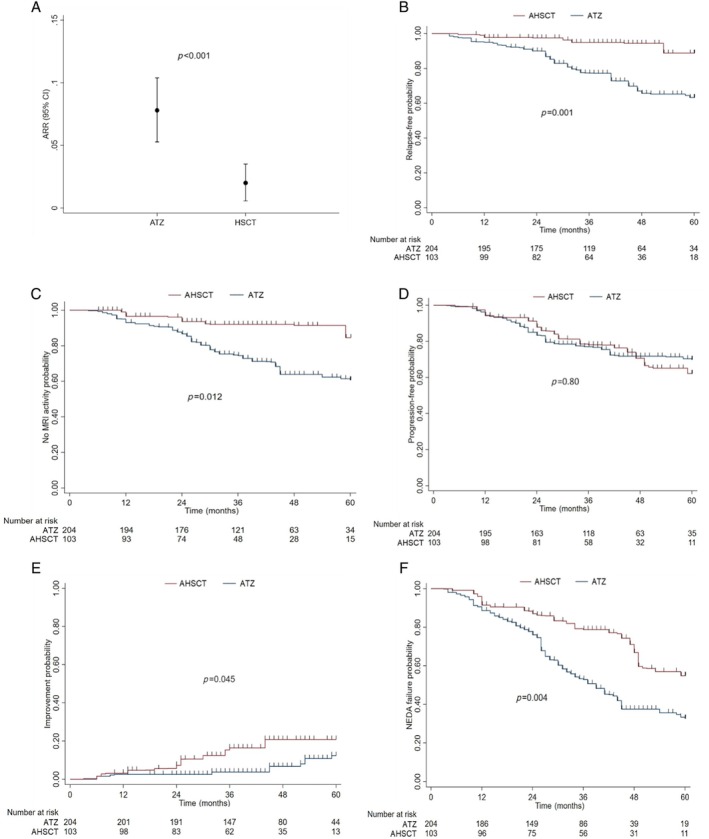
Figure 3: Stem cells vs. Ocrevus