Article responses on hsct?
Re: Article responses on hsct?
At first the group is not very representative - EDSS average 6,0, all but one SPMS or PPMS.
What is interesting is data about inflammation - if the inflammation is seen, the effectiveness is quite impressive, without inflammation its rather problematic.
To asses it fully I would like to know how far this disease went in those unlucky patients, because someone cant be classified as disease free progression, because his EDSS went up by 1,0 after 10 years, but I will buy such progression at any time ;)
Of course, 25% seems rather disappointing comparing to what we hope HSCT to be , but still, not going into details, methods and so on - anyone heard about scientific research that proved any method that gave 25% of MSers 15 years without detoriation? And we are talking here about PPMS -from what I know there is no cure registered drug/medicament for PPMS.
The point about inflammation I think can be really important - I have no doubts that MS is thing of immunology, but I think after some time the role of immunity decreases in MS, the neurodegeneration goes on without ignition of immunology. Trying to draw some colourful analogy - curing longlived MS is like fortyfying the town after having some troops already inside. We really do not know a thing about how the neurodegeneration process without inflammation works. We know only thats it is really hard to cure it (RRMS in fact isnt also the example of easiest ;)
Sorry for my english, I am not native speaker and not even using english in everyday life.
What is interesting is data about inflammation - if the inflammation is seen, the effectiveness is quite impressive, without inflammation its rather problematic.
To asses it fully I would like to know how far this disease went in those unlucky patients, because someone cant be classified as disease free progression, because his EDSS went up by 1,0 after 10 years, but I will buy such progression at any time ;)
Of course, 25% seems rather disappointing comparing to what we hope HSCT to be , but still, not going into details, methods and so on - anyone heard about scientific research that proved any method that gave 25% of MSers 15 years without detoriation? And we are talking here about PPMS -from what I know there is no cure registered drug/medicament for PPMS.
The point about inflammation I think can be really important - I have no doubts that MS is thing of immunology, but I think after some time the role of immunity decreases in MS, the neurodegeneration goes on without ignition of immunology. Trying to draw some colourful analogy - curing longlived MS is like fortyfying the town after having some troops already inside. We really do not know a thing about how the neurodegeneration process without inflammation works. We know only thats it is really hard to cure it (RRMS in fact isnt also the example of easiest ;)
Sorry for my english, I am not native speaker and not even using english in everyday life.
- georgegoss
- Family Elder
- Posts: 284
- Joined: Sat Oct 30, 2010 2:00 pm
- Location: California
- Contact:
Re: Article responses on hsct?
czapski hit the nail on the head and correctly mentions the issue that I did not, but should have in my original explanation. The treated group of patients in the Greek study were also predominantly advanced progressive (both PP and SP) cases that were not ambulatory (EDSS range 6.0-8.0). Again, these are the patients that are known to respond "least" favorably to HSCT treatment. So many of these people never experienced a stopping of their disease activity at all, even from the very begining immediately following HSCT. So these "failed treatment" patients were included in the 15 year follow up numbers. From a statistical perspective that really skews the numbers and makes the wrong argument that "HSCT does not have long term benefit." Which is an absurdly false statement.
In actuality for HSCT treatment for MS patients since 2002, for every single patient that had their MS disease stopped, all (100%) of these same patients still have their disease stopped today. That's 100% effectiveness at 10 years out. A far different way to look at the data compared to the Greek study, even though both data are correct. It's all the way the data is presented and interpreted. Like Samuel Clemmons said. . . . "Lies, damn lies and statistics." So the lesson here is manifold. . . . Treatment earier in the disease lifecycle is more effective and treatment of patients while still ambulatory is more effective. Without digging further and depper into the Greek presentation and just looking superficially at the data I can see how some people could become discouraged by the data. But I rather look at the details to get the "real" story, which is this. . . .
The specific statistical "probability" that has been demonstrated for each morphological evolution groups (RR, SP, PP) for halting of underlying disease activity is as follows:
Ealy RRMS-treated patients
Complete stopping of the disease process & progression in virtually 100% of treated patients.
Greater than 80% of the same treatment population experiences "significant" improvement (>1.0 point reduction of existing symptomatic EDSS). Many HSCT-treated patients in this group further report their pre-treatment symptoms completey dissappearing, 100%.
During the RRMS phase of the disease I would expect very good beneficial results following HSCT regardless of the EDSS-measured symptomatic disability at the time of treatment (highly effective in the entire EDSS range).
Late SPMS (non ambulatory) treated patients
Stopping of MS disease progression in 78% of this treatment population.
EDSS improvement not population-quantified in this population and varies by individual.
Curative efficacy is not population-quantified in other patient EDSS stratum. So for SPMS patients with an ambulatory status (EDSS <6.0), the cure rate (stopping of diasease progression) is not well established, but certainly I would expect it to be greater than 78%. Probably in the range of 85% - 95%.
Just my own personal expeience data point (that does not necessarily translate to any other specific individual) that appears to be consistent and fairly representative of other (ambulatory) SPMS patients so far. . . . . I was RRMS for 11 years and then went SPMS for 4 years (EDSS 3.5) before my HSCT procedure. As of today (18 months post-transplantation) my disease is 100% stopped and my pre-existing symptomatic deficit (as measured by EDSS) has improved (reversed) 50%. So clearly it is possible that SPMS cases (especially those that are ambulatory) can experience good beneficial improvement from HSCT.
Late PPMS (non ambulatory) treated patients
Stopping of MS disease progression in 66% of this treatment population.
EDSS improvement likely poor, if at all
So for the PPMS patients with an ambulatory status (EDSS <6.0), the cure rate (stopping of disease progression) is not well studied and not well established, but certainly I would expect it to be greater than 66% people in the PPMS population.
Also, for ambulatory PPMS cases, EDSS improvement is possible, but not gauranteed. This is a very un-studied and unknown area. I would expect this number of people in this poulation to show improvement somewhere in the chasm-like range of 1% - 65% of treated patients. Perhaps someday as more ambulatory PPMS patients are treated then this can be better quantified. For now, the treated population is so small its impossible to predict with any confidence.
But no matter what, HSCT has a far better chance of having a positve beneficial effect for MS patients of any evolutionary type as compared to any (every) other therapy anywhere in the world. So far, no other curative therapy can even come close in accomplishing what HSCT has already (scientifically and repeatably) demonstrated.
Here is a single graph that I created that provides a comparative overview of all the aforementioned data:
http://2.bp.blogspot.com/-PvejGH-NIG4/T ... al%2B2.jpg
In actuality for HSCT treatment for MS patients since 2002, for every single patient that had their MS disease stopped, all (100%) of these same patients still have their disease stopped today. That's 100% effectiveness at 10 years out. A far different way to look at the data compared to the Greek study, even though both data are correct. It's all the way the data is presented and interpreted. Like Samuel Clemmons said. . . . "Lies, damn lies and statistics." So the lesson here is manifold. . . . Treatment earier in the disease lifecycle is more effective and treatment of patients while still ambulatory is more effective. Without digging further and depper into the Greek presentation and just looking superficially at the data I can see how some people could become discouraged by the data. But I rather look at the details to get the "real" story, which is this. . . .
The specific statistical "probability" that has been demonstrated for each morphological evolution groups (RR, SP, PP) for halting of underlying disease activity is as follows:
Ealy RRMS-treated patients
Complete stopping of the disease process & progression in virtually 100% of treated patients.
Greater than 80% of the same treatment population experiences "significant" improvement (>1.0 point reduction of existing symptomatic EDSS). Many HSCT-treated patients in this group further report their pre-treatment symptoms completey dissappearing, 100%.
During the RRMS phase of the disease I would expect very good beneficial results following HSCT regardless of the EDSS-measured symptomatic disability at the time of treatment (highly effective in the entire EDSS range).
Late SPMS (non ambulatory) treated patients
Stopping of MS disease progression in 78% of this treatment population.
EDSS improvement not population-quantified in this population and varies by individual.
Curative efficacy is not population-quantified in other patient EDSS stratum. So for SPMS patients with an ambulatory status (EDSS <6.0), the cure rate (stopping of diasease progression) is not well established, but certainly I would expect it to be greater than 78%. Probably in the range of 85% - 95%.
Just my own personal expeience data point (that does not necessarily translate to any other specific individual) that appears to be consistent and fairly representative of other (ambulatory) SPMS patients so far. . . . . I was RRMS for 11 years and then went SPMS for 4 years (EDSS 3.5) before my HSCT procedure. As of today (18 months post-transplantation) my disease is 100% stopped and my pre-existing symptomatic deficit (as measured by EDSS) has improved (reversed) 50%. So clearly it is possible that SPMS cases (especially those that are ambulatory) can experience good beneficial improvement from HSCT.
Late PPMS (non ambulatory) treated patients
Stopping of MS disease progression in 66% of this treatment population.
EDSS improvement likely poor, if at all
So for the PPMS patients with an ambulatory status (EDSS <6.0), the cure rate (stopping of disease progression) is not well studied and not well established, but certainly I would expect it to be greater than 66% people in the PPMS population.
Also, for ambulatory PPMS cases, EDSS improvement is possible, but not gauranteed. This is a very un-studied and unknown area. I would expect this number of people in this poulation to show improvement somewhere in the chasm-like range of 1% - 65% of treated patients. Perhaps someday as more ambulatory PPMS patients are treated then this can be better quantified. For now, the treated population is so small its impossible to predict with any confidence.
But no matter what, HSCT has a far better chance of having a positve beneficial effect for MS patients of any evolutionary type as compared to any (every) other therapy anywhere in the world. So far, no other curative therapy can even come close in accomplishing what HSCT has already (scientifically and repeatably) demonstrated.
Here is a single graph that I created that provides a comparative overview of all the aforementioned data:
http://2.bp.blogspot.com/-PvejGH-NIG4/T ... al%2B2.jpg
Re: Article responses on hsct?
From everything that I have read, this is true. At some point in time inflamation ceases and then neurodegeneration is predominant. One theory is that when enough of the meylin sheath is destroyed the axons are exposed and begin to degenerate. This is due to the fact that the health of the axon is dependant on nerve growth factors that are available at the interface of the meylin and axon (the part of the meylin that contacts the axon).The point about inflammation I think can be really important - I have no doubts that MS is thing of immunology, but I think after some time the role of immunity decreases in MS, the neurodegeneration goes on without ignition of immunology.
I posted this before, but here is a good article that describes this:
http://www.jhasin.com/files/articlefile ... p37_41.pdf
So I think that the important thing with HSCT in my mind would be to cease disease progression before the swtich between inflamation and neurodegeneration happens. Not to say that HSCT does not help people with SPMS or PPMS becuase I think that once the disease process is stopped, remeylination can occur.
Re: Article responses on hsct?
Thank you George, this brings order to the chaos!
- georgegoss
- Family Elder
- Posts: 284
- Joined: Sat Oct 30, 2010 2:00 pm
- Location: California
- Contact:
Re: Article responses on hsct?
You bring up some good points CV. But the assertion that axonal dystrophy (neurodegeneration) follows myelin destruction may sometimes be true, but not always.
Take PPMS cases as example. Pimary progressive cases immediately enter a pathology of axonal dystrophy without much evidence of isolated myelin destruction. So if the statement of "the neurodegeneration goes on without ignition of immunology," then why does HSCT work to stop the progression of PPMS in fully more than two-thirds of patients? If immunity were not involved, then ablating autoreactive lymphocytes should otherwise have 0% beneficial effect. But this has not been shown to be the case.
This also makes me think of the question as to why do the majority of RRMS cases eventually transition into SPMS (such as my own history)? The answer to both of these progressive MS disease morphology (PP and SP) questions remains a mystery, as does the underlying etiological cause of MS in general. I suspect that once the root cause of MS is discovered, probably it will simultaneously be discovered why progressive cases manifest.
Take PPMS cases as example. Pimary progressive cases immediately enter a pathology of axonal dystrophy without much evidence of isolated myelin destruction. So if the statement of "the neurodegeneration goes on without ignition of immunology," then why does HSCT work to stop the progression of PPMS in fully more than two-thirds of patients? If immunity were not involved, then ablating autoreactive lymphocytes should otherwise have 0% beneficial effect. But this has not been shown to be the case.
This also makes me think of the question as to why do the majority of RRMS cases eventually transition into SPMS (such as my own history)? The answer to both of these progressive MS disease morphology (PP and SP) questions remains a mystery, as does the underlying etiological cause of MS in general. I suspect that once the root cause of MS is discovered, probably it will simultaneously be discovered why progressive cases manifest.
Re: Article responses on hsct?
George,
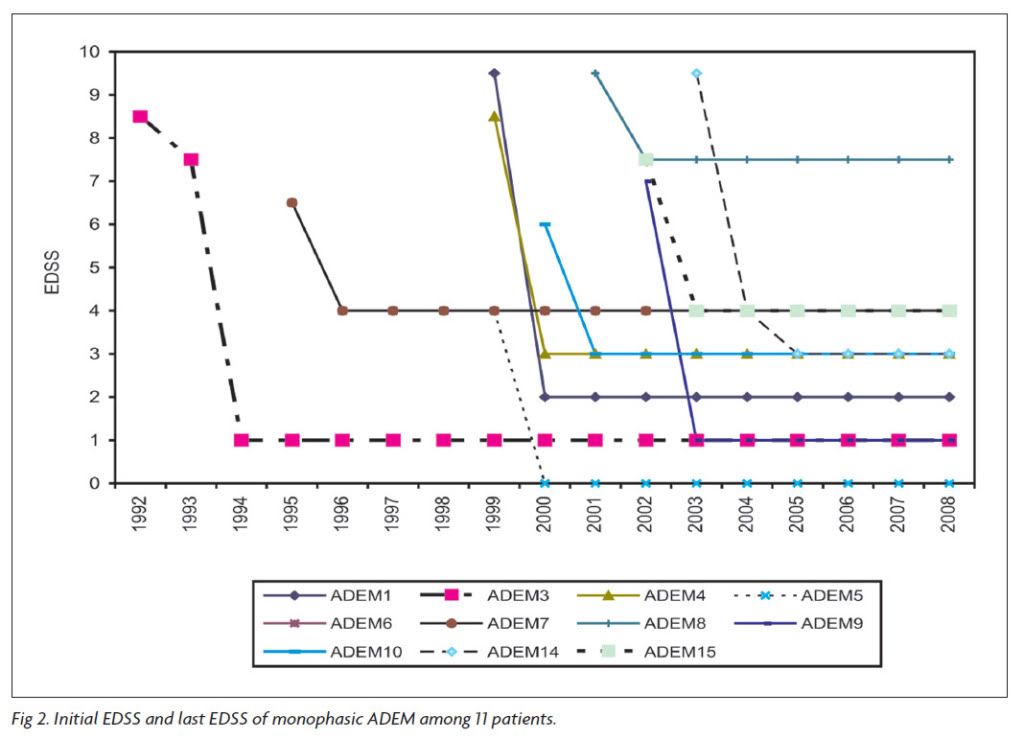
Yes, I could be totally wrong about inflamation and neurodegeneration but let me give you some of my experience as someone who has had ADEM which many scientists think is related to MS.
So, when I went into the hospital I had severe syptoms such as double vision, headache, vomiting and eventually a grand mal seizure. While in the hospital I had a full series of MRI's of both my brain and spine and they were all normal.
This phenomena of having severe attacks and normal MRI is not that uncommon in people with ADEM:
http://www.ncbi.nlm.nih.gov/pubmed/11415907
Interesting though, ADEM attacks a person and then it can be stopped. I look at it as a mistake in the immune system that can be reversed. But even though it can be stopped, severe disability occurrs and then some recovery can be obtained once it is stopped (I went from an EDSS of 7 to 4 where I am now). Here is a good graph showing this:
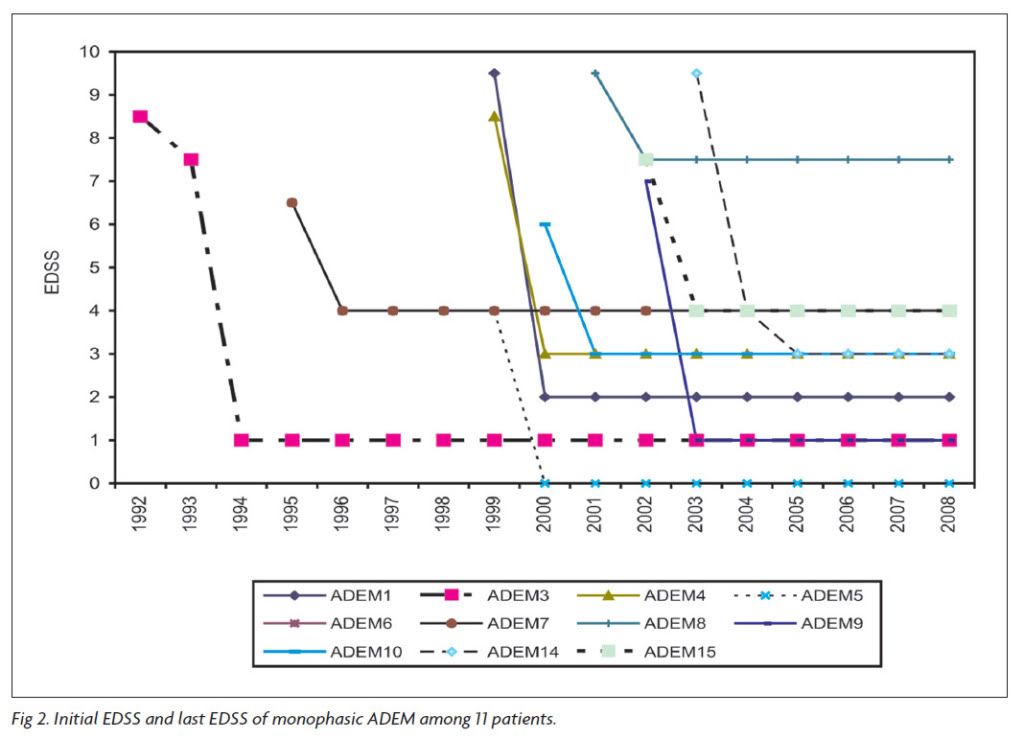
So, it appears that neurodegeneration can happen in ADEM without much evidence of it, at least initially. My thought is that maybe in primary progressive MS, inflamation occurs quickly to the point where the axons are exposed but then the inflamation is halted and neurodegeneration continues.
Personally, I think PPMS and RRMS/SPMS are distinct from each other.
Yes, I could be totally wrong about inflamation and neurodegeneration but let me give you some of my experience as someone who has had ADEM which many scientists think is related to MS.
So, when I went into the hospital I had severe syptoms such as double vision, headache, vomiting and eventually a grand mal seizure. While in the hospital I had a full series of MRI's of both my brain and spine and they were all normal.
This phenomena of having severe attacks and normal MRI is not that uncommon in people with ADEM:
http://www.ncbi.nlm.nih.gov/pubmed/11415907
So it appears that damage can occur (at least in ADEM) without any appearance of inflamation, or the imflamation may be missed due to sampling error. My guess is that PPMS and ADEM have some paralells.BACKGROUND AND PURPOSE: White matter lesions on MR images obtained from patients with acute disseminated encephalomyelitis (ADEM) have been reported to appear shortly after symptom onset, and their resolution has been claimed to parallel recovery. To elucidate the temporal evolution of these lesions and to associate the changes on MR images to the patients' clinical condition, we performed serial MR imaging on patients with ADEM.
CONCLUSION: MR imaging performed during the first days after the onset of the disease may not reveal any pathologic findings. The appearance of the ADEM-associated MR imaging changes may be associated with recovery rather than decline. It remains to be studied whether the new MR imaging techniques reveal the lesions associated with ADEM faster than the conventional T2-weighted imaging.
Interesting though, ADEM attacks a person and then it can be stopped. I look at it as a mistake in the immune system that can be reversed. But even though it can be stopped, severe disability occurrs and then some recovery can be obtained once it is stopped (I went from an EDSS of 7 to 4 where I am now). Here is a good graph showing this:
So, it appears that neurodegeneration can happen in ADEM without much evidence of it, at least initially. My thought is that maybe in primary progressive MS, inflamation occurs quickly to the point where the axons are exposed but then the inflamation is halted and neurodegeneration continues.
Personally, I think PPMS and RRMS/SPMS are distinct from each other.
- georgegoss
- Family Elder
- Posts: 284
- Joined: Sat Oct 30, 2010 2:00 pm
- Location: California
- Contact:
Re: Article responses on hsct?
CV. . . I really like the way you present valid and compelling data. Makes total sense.
I find it fascinating that the disability trend as you have presented for ADEM is generally inverted as compared to the upward trend in progressive MS cases. And although this trend is not the same for ADEM and MS, it does seem that there must be some possible related activity in one that might shed light on the other. Anyway, what you present here makes me think about, and want to learn more about this subject that I know so little about.
Personally, I think PPMS and RRMS/SPMS are distinct from each other.
You certainly are not alone in this opinion. There are many doctors that are of the same view.
I have no specific interest that the etiological cause be one thing, or another. I just hope for the soonest discovery of the actual cause (whatever it is) so that we can beat both of these diseases. Thanks very much for bringing these discussion points to the table.
I find it fascinating that the disability trend as you have presented for ADEM is generally inverted as compared to the upward trend in progressive MS cases. And although this trend is not the same for ADEM and MS, it does seem that there must be some possible related activity in one that might shed light on the other. Anyway, what you present here makes me think about, and want to learn more about this subject that I know so little about.
Personally, I think PPMS and RRMS/SPMS are distinct from each other.
You certainly are not alone in this opinion. There are many doctors that are of the same view.
I have no specific interest that the etiological cause be one thing, or another. I just hope for the soonest discovery of the actual cause (whatever it is) so that we can beat both of these diseases. Thanks very much for bringing these discussion points to the table.
Re: Article responses on hsct?
CV and George,
thanks for everything you've just written and it does make a lot of sense. although, my science background is minimal, so my 'sense' is not the same as yours! therefore, you're putting some sense into me!
therefore, you're putting some sense into me!
thanks for everything you've just written and it does make a lot of sense. although, my science background is minimal, so my 'sense' is not the same as yours!
Re: Article responses on hsct?
Yes there are a lot of simlilarities in ADEM and MS. In fact about 30% of people with ADEM end up transitioning to MS (first through recurrent ADEM) which seems to be where I am going. After being in a wheel chair I can say I am going to try everything I can stop progression and HSCT gives a lot of hope to many.I find it fascinating that the disability trend as you have presented for ADEM is generally inverted as compared to the upward trend in progressive MS
cases. And although this trend is not the same for
ADEM and MS, it does seem that there must be
some possible related activity in one that might
shed light on the other.
Re: Article responses on hsct?
The main reason I posted the article was the startling differences in the progression rates in the study compared to what I have read elsewhere. I always learn a ton when you science guys get rolling on these topics. It is always. Good to see Dave around TIMS. I know I am coming in late (work has been ridiculous this month) but thanks for all of the input guys.
"A gun is a tool, Marian; no better or no worse than any other tool: an axe, a shovel or anything. A gun is as good or as bad as the man using it. Remember that." -- Shane
Who is John Galt?
Who is John Galt?
- ActiveMSers
- Family Member
- Posts: 27
- Joined: Tue Jul 25, 2006 2:00 pm
- Contact:
Re: Article responses on hsct?
George, I believe you are mistaken. Total Body Irradiation was not part of this study's protocol. In fact, two thirds received a form of BEAM, today's primary HSCT for MS treatment, making the Greek study quite relevant. The primary reason why researchers are focused on RRMS and less on SPMS (and not on PPMS) was highlighted in this trial. "Only 10% of patients who went into the study without evidence of ongoing inflammation were able to remain disease free." People in the RRMS stage of this disease typically have active lesions, although it is common in the earlier stages of SPMS as well. Anyone who is seriously considering this treatment would be advised to spend the $30 to read this study in full.georgegoss wrote:This early Greek HSCT study used a protocol that is no longer used for treatment of MS. Mainly that they incorporated Total Body Irradiation (TBI) as part of the treatment protocol.
I am a strong proponent of HSCT for MS and have just returned from a week of 2-year post transplant testing for my trial. I hope to have a full update posted at ActiveMSers in the coming days.
-Dave
Re: Article responses on hsct?
When I met with dr Burt, they told me that I didn't have any active lesions, but the lesion load has increased substantially, so I guess the inflammatory stage can be diagnosed in either of those ways.
"A gun is a tool, Marian; no better or no worse than any other tool: an axe, a shovel or anything. A gun is as good or as bad as the man using it. Remember that." -- Shane
Who is John Galt?
Who is John Galt?