drsclafani wrote:Cece wrote: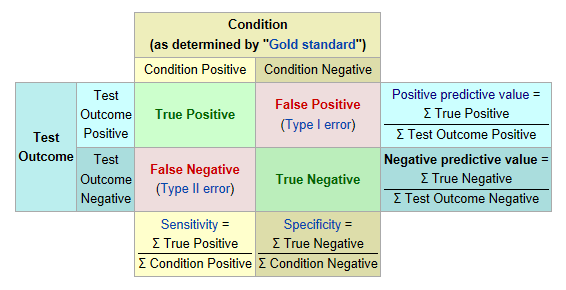
cece
your turn, explain that in english for everyonoe
If I knew it in english, I might not have had to go looking for a chart!
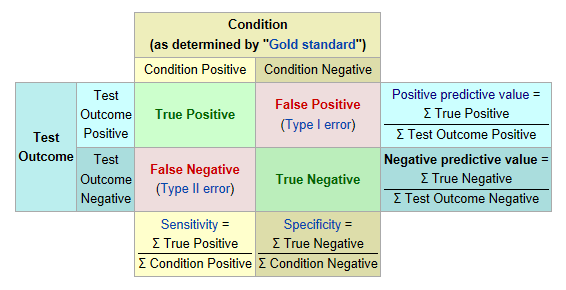
At the top it says, "Condition (as determined by the gold standard)," in the tan box. We are discussing the condition of CCSVI. We are in agreement that the gold standard is venogram plus ivus. Venogram plus ivus shows the truth, as best we can determine it. The left column, "Condition Positive," means that a patient truly has a blocked vein. The right column, "Condition negative," means the patient truly does not have a blocked vein.
In my own case, the gold standard of venogram plus ivus showed jugular stenoses in both jugulars but nothing in the azygous vein. I truly had bilateral jugular stenosis.
On the left, in a blue box, it says, "Test outcome." Some possible tests in CCSVI are doppler ultrasound, MRV, Haacke protocol MRV, plethysmography, and I recently read a post from someone who had their neck pinched in an attempt to feel the jugular and determine a stenosis.
Not all these tests are going to show the right answers.
The top row is for patients who had their test outcomes show positive. The doppler shows CCSVI, or the MRV showed CCSVI, or the pinch test showed CCSVI. This may or may not be the truth, but it is what the test shows. If it really is the truth, they land in the 'true positive' green square. But if it is not the truth, then they land in the 'false positive' pink square.
My doppler prior to my procedure showed that I had CCSVI (3 criteria met). Venogram plus ivus confirmed this. I truly had CCSVI and my test had showed this, so that was a true positive.
A patient posted recently, about his continuing search for answers. I hope it is ok to remember that his doppler had showed CCSVI, but when he went in for the venogram plus ivus, there was no CCSVI. His veins looked great. His test had been a false positive.
Take the total number of true positives and divide them by test outcome positives and you have the positive predictive value. It's interesting that in CCSVI, the number of true positives is very high if looking exclusively at patients with MS. Out of 100 patients with MS, the venogram plus ivus combination will show CCSVI in approximately 99 or 100 of them. Let's say 99 out of 100 are true positives. Let's say the doppler identified CCSVI in 90 of them. The positive predictive value would be 99 divided by 90, which comes to 1.1 or 110%. It looks as if the doppler is excellent at identifying patients who will have CCSVI. But then again, the simple question of asking, "Do you have MS?" is equally excellent at identifying who will have CCSVI.
All right, on to the next row. These are the patients who have had a test for CCSVI and, tears and distress, it came up negative. We have heard from patients who accept that and give up on pursuing CCSVI. And we have heard from patients who do not accept the negative test and go on to get a venogram done. If the doppler said there was no CCSVI but the truth as seen using venogram plus ivus is that the patient truly has CCSVI, then they land in the false negative square. If, sadly, the test showed no CCSVI and the venogram plus ivus showed no CCSVI, then they land in the true negative column. I would have to check back but I believe there have been some patients with Parkinsons or nonMS disorders that were true negatives. No CCSVI found, no CCSVI to treat, nothing gained except the knowledge that this is not the answer, for them.
Take the number of true negatives and divide by the total number of negatives and you get the negative predictive value. Let's say the doppler identified CCSVI in 90 out of 100 patients, so we'll take the 10 that were negative according to the test, and check them with venogram plus ivus, and 9 of them were false negatives (because they truly had CCSVI) but one was a true negative. 1 true negative divided by 10 test outcome negatives means the doppler has a negative predictive value of 10%. That's pretty bad.
(Explaining in plain english takes forever! But we are getting near the end now.)
The sensitivity square is at the bottom of the first column, which is the 'condition positive' column. Take the number of true positives divided by the number of condition positives? Ok... 99 out of 100 pwMS truly have CCSVI as shown by venogram plus ivus, going by the numbers I've used thus far. That's the bottom number, the number of condition positives. The doppler identified 90 out of 100 as having CCSVI, so it didn't get them all, but pretty good. 90 is the top number, the number of 'true positives' identifiable by the test. 90 divided by 99 comes out to 91%. Sensitivity is 91%. I don't know what to compare that to but it seems like a high sensitivity to me.
Next column, we've got the specificity square. The number of 'true negatives' as identified by the test needs to be divided by the number of 'condition negatives'? In my example, we had one true negative (because CCSVI is almost overwhelmingly found in pwMS both by doppler and by venogram plus ivus.) And in my example, the doppler correctly found that one true negative, even though it also identified nine others as negatives when they really weren't, but that part is addressed with the negative predictive power row, and this is the specificity column. So 1 true negative divided by 1 condition negative gives a specificity of 100%. Perfect specificity.
The big problem with the doppler was not the specificity or the sensitivity or the positive predictive power. The big problem was the negative predictive power, at 10%.
And when we hear references to venogram as the 'tarnished' gold standard, that is not good! If the gold standard does not represent the true truth, then the calculations will be off. There have not yet been any studies using venogram plus ivus as the gold standard.
Ok, that's my best attempt at plain english, if not concise english.