DrSclafani answers some questions
Re: DrSclafani answers some questions
Learning points
1.Stents can remain patent for many years without migration but with some compression. Stenosis can be both in-stent restenosis and external compression, as we have seen today.
2. Periodic management of these in-stent restenoses is relatively simple.
3. It took three venograms and two IVUS before an azygous arch stenosis was discovered.
4. A nutcracker syndrome was not considered by two prior angiographers.
5. We have seen and recognized the mastoid emissary veins for the first time
6. Septums are very difficult to treat. Balloon angioplasty just compresses it back up against the wall of the vein.
Thanks Dr S this is fantastic, only people with eyes a brain and balls or courage would stand up and say it as it is.
The ups and downs and the failings all have to be out there. None of us will learn and achieve the best outcome without this honesty.
FANTASTIC effort,
** Now I have a question, will repeated treatments be less common if IVUS was used by an operator with equal or better skill to yourself at the first assessment?
** It appears the use of stents are going to be a statistical issue because of the choice to use them in early procedures. Some of the follow up testing needs to be timed to the healing process to maximise the flow when using stents. The follow up and 'watching the progress' as the body adjusts to the stent is vital. Will there need to be a second procedure to minimise the thrombosis/ clotting/ natural healing effect when stents are used and in particular cases will need to be observed with IVUS?
** Have you found a pattern of IVUS findings that give you and indication as to what will be a one time event and what will require more than one treatment? For example if the finding is immobile valve compared with a septum? If there is need to use a stent, what is the likelihood of re-treatment?
Thanks,
Nigel
1.Stents can remain patent for many years without migration but with some compression. Stenosis can be both in-stent restenosis and external compression, as we have seen today.
2. Periodic management of these in-stent restenoses is relatively simple.
3. It took three venograms and two IVUS before an azygous arch stenosis was discovered.
4. A nutcracker syndrome was not considered by two prior angiographers.
5. We have seen and recognized the mastoid emissary veins for the first time
6. Septums are very difficult to treat. Balloon angioplasty just compresses it back up against the wall of the vein.
Thanks Dr S this is fantastic, only people with eyes a brain and balls or courage would stand up and say it as it is.
The ups and downs and the failings all have to be out there. None of us will learn and achieve the best outcome without this honesty.
FANTASTIC effort,
** Now I have a question, will repeated treatments be less common if IVUS was used by an operator with equal or better skill to yourself at the first assessment?
** It appears the use of stents are going to be a statistical issue because of the choice to use them in early procedures. Some of the follow up testing needs to be timed to the healing process to maximise the flow when using stents. The follow up and 'watching the progress' as the body adjusts to the stent is vital. Will there need to be a second procedure to minimise the thrombosis/ clotting/ natural healing effect when stents are used and in particular cases will need to be observed with IVUS?
** Have you found a pattern of IVUS findings that give you and indication as to what will be a one time event and what will require more than one treatment? For example if the finding is immobile valve compared with a septum? If there is need to use a stent, what is the likelihood of re-treatment?
Thanks,
Nigel
Re: DrSclafani answers some questions
Hi Doc,
Very impressive case, i wish more docs approached ccsvi like you do...
Robert
Very impressive case, i wish more docs approached ccsvi like you do...
Robert
Re: DrSclafani answers some questions
what a case all in one and what an investigation by our dr-prof. Sclafani
i hope she will manage to improve her situation.
how many things you gave us with the last two cases!!!
thank you DR Sclafani,for everything you are doing for everyone of us msers and ccsviers
agni
i hope she will manage to improve her situation.
how many things you gave us with the last two cases!!!
thank you DR Sclafani,for everything you are doing for everyone of us msers and ccsviers
agni
- drsclafani
- Family Elder
- Posts: 3182
- Joined: Fri Mar 12, 2010 3:00 pm
- Location: Brooklyn, New York
- Contact:
Re: DrSclafani answers some questions
Nigel, it is always easier to share other doctors problems, failing and complications than my own. That is not to say that I do not have complications. It is more difficult to speak about my own complications for their medicolegal consequences. Sad but true. Nonetheless, it should be mentioned that both of the doctors who treated this patient are impressive, scholarly and technically adept.NZer1 wrote:
Thanks Dr S this is fantastic, only people with eyes a brain and balls or courage would stand up and say it as it is.
The ups and downs and the failings all have to be out there. None of us will learn and achieve the best outcome without this honesty.
FANTASTIC effort,
Thanks,
Nigel
I would suggest that it is the inquiring minds that push this forward and I thank all the readers and responders who have pushed my envelope for me. For example, the question yesterday about steroids and healing of the venoplasty. Brilliant! ...I didnt know the answer. i sought the information and i am better for it now. Thanks...and keep pushing.
Salvatore JA Sclafani MD
Patient contact: ccsviliberation@gmail.com
Patient contact: ccsviliberation@gmail.com
- drsclafani
- Family Elder
- Posts: 3182
- Joined: Fri Mar 12, 2010 3:00 pm
- Location: Brooklyn, New York
- Contact:
Re: DrSclafani answers some questions
I think that IVUS adds much to this examination. It should help any operator who learns to use it properly.NZer1 wrote:
FANTASTIC effort,
** Now I have a question, will repeated treatments be less common if IVUS was used by an operator with equal or better skill to yourself at the first assessment?
I would manage patients who come to me by evaluating the process. Some of these stents are not as successful as this one. Some patients have inadequate response and follow-up imaging, initially with noninvasive methods and then with venography, is extremely important.** It appears the use of stents are going to be a statistical issue because of the choice to use them in early procedures. Some of the follow up testing needs to be timed to the healing process to maximise the flow when using stents. The follow up and 'watching the progress' as the body adjusts to the stent is vital. Will there need to be a second procedure to minimise the thrombosis/ clotting/ natural healing effect when stents are used and in particular cases will need to be observed with IVUS?
IVUS is very important in evaluating stents. In-stent restenosis (ISR) is optimally visualized by IVUS. imaging immediately after treatment of ISR allows good visualization of the lumen and determines better than venography the dimensions of the lumen.
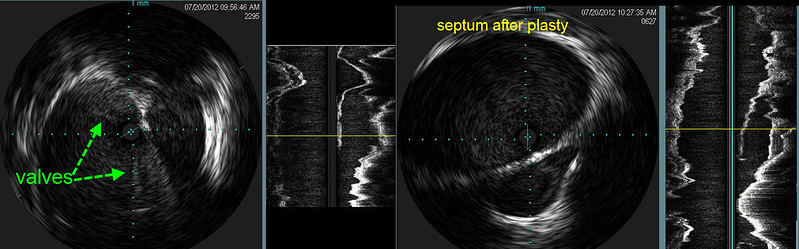
I think that septum is better visualized by IVUS than by venography. Venographic appearance of septum looks similar to opacification of the vein below the valve when the contrast jets through the obstruction. But either way, treatment of septum is unclear, both regarding the need to treat or the method of treatment. If it is found to be truly an impediment to flow, then we need to figure out how to treat it, for balloon angioplasty does not seem to work.** Have you found a pattern of IVUS findings that give you and indication as to what will be a one time event and what will require more than one treatment? For example if the finding is immobile valve compared with a septum? If there is need to use a stent, what is the likelihood of re-treatment?Thanks,
Nigel
it appears to me that retreatment prediction is not quite ready for prime time. For the moment, and probably forever, retreatment will be determined by clinical response to the treatment.
Salvatore JA Sclafani MD
Patient contact: ccsviliberation@gmail.com
Patient contact: ccsviliberation@gmail.com
Re: DrSclafani answers some questions
Hi Dr. Sclafani,
Thanks for sharing this terrific case with us.
Here's an MRV image some readers might like to see:

Right lateral view of the craniocervical junction in a venous corrosion cast. Note the presence of a prominent mastoid emissary vein (n) connecting to a deep cervical vein (m). The carotid artery venous plexus is clearly visible (l). b, transverse sinus; d, cavernous sinus; c, sigmoid sinus; a, superior jugular bulb; v, pterygoid plexus; g, posterior condylar vein; h, lateral condylar vein; u, internal jugular vein.
This and other MRV images are here: http://www.ajnr.org/content/23/9/1500.full
Thanks for sharing this terrific case with us.
Here's an MRV image some readers might like to see:

Right lateral view of the craniocervical junction in a venous corrosion cast. Note the presence of a prominent mastoid emissary vein (n) connecting to a deep cervical vein (m). The carotid artery venous plexus is clearly visible (l). b, transverse sinus; d, cavernous sinus; c, sigmoid sinus; a, superior jugular bulb; v, pterygoid plexus; g, posterior condylar vein; h, lateral condylar vein; u, internal jugular vein.
This and other MRV images are here: http://www.ajnr.org/content/23/9/1500.full
Last edited by HappyPoet on Wed Jul 25, 2012 12:16 pm, edited 1 time in total.
Re: DrSclafani answers some questions
How common is the use of high pressure balloons? I remember you doing a survey of other IRs back around SIR or ISNVD time, was that one of the questions asked?drsclafani wrote:I find it uncommon for patients to require stents during the first treatment. Most of the time, the stenoses, commonly caused by immobile valves, are readily opened by use of high pressure fairly large balloons.
She had another venogram with IVUS in 2011. At that time both internal jugular veins underwent double balloon angioplasty . Some treatment of the azygous vein was also undertaken. The entire procedure was said to have lasted about 30 minutes.
My own first procedure was about as quick as a procedure could be and that was an hour and fifteen minutes, with IVUS. Thirty minutes does not seem possible, especially considering that IVUS adds time to the procedure.
However after conception of her first child, these benefits regress.
Unfortunately, her gains were lost during her second pregnancy.
Is pregnancy known to contribute to restenosis in any other venous diseases?
When there is external compression of a stent by bone, will it continue to worsen over time, or can it be expected to be stable at the degree of narrowing that it is at?
(great image, it's striking how high the stents are, and the narrowing in the orange circle is concerning and easy to see)
IVUS before (left 2 images) showed that there were immobile incompletely opening thickened valves (green arrows) and a fluid containing area to the right of the jugular vein. The next image is a longitudinal view and one can clearly see the blind ending sac outlined by thickened tissue representing a septum. IVUS after angioplasty (right 2 images) showed that the valve is opened but there is no change in the septum.
wow, it didn't change the septum at all
Re: DrSclafani answers some questions
In the first image, it could be mistaken for a healthy vein because the width looks good. The shade of contrast in the septum is lighter but subtle. In the second image it is clear from your labeling how narrow the opening gets but if you had shown us the image out of context, I would not have known what we were seeing.The outpocketing of contrast media to the left of the internal jugular vein represents contrast extending into the septum. To prove it I placed a catheter into the orifice of this septum (orange arrow). After balloon angioplasty the contrast column is smoother and the flow was faster but the bulge has changed little.
- drsclafani
- Family Elder
- Posts: 3182
- Joined: Fri Mar 12, 2010 3:00 pm
- Location: Brooklyn, New York
- Contact:
Re: DrSclafani answers some questions
Great! Thanks!HappyPoet wrote:Hi Dr. Sclafani,
Thanks for sharing this terrific case with us.
Here's an MRV image some readers might like to see:
Right lateral view of the craniocervical junction in a venous corrosion cast. Note the presence of a prominent mastoid emissary vein (n) connecting to a deep cervical vein (m). The carotid artery venous plexus is clearly visible (l). b, transverse sinus; d, cavernous sinus; c, sigmoid sinus; a, superior jugular bulb; v, pterygoid plexus; g, posterior condylar vein; h, lateral condylar vein; u, internal jugular vein.
This and other MRV images are here: http://www.ajnr.org/content/23/9/1500.full
i have been speaking to Dr Schelling about these emissary veins and he is most knowledgeable about them.
Salvatore JA Sclafani MD
Patient contact: ccsviliberation@gmail.com
Patient contact: ccsviliberation@gmail.com
Re: DrSclafani answers some questions
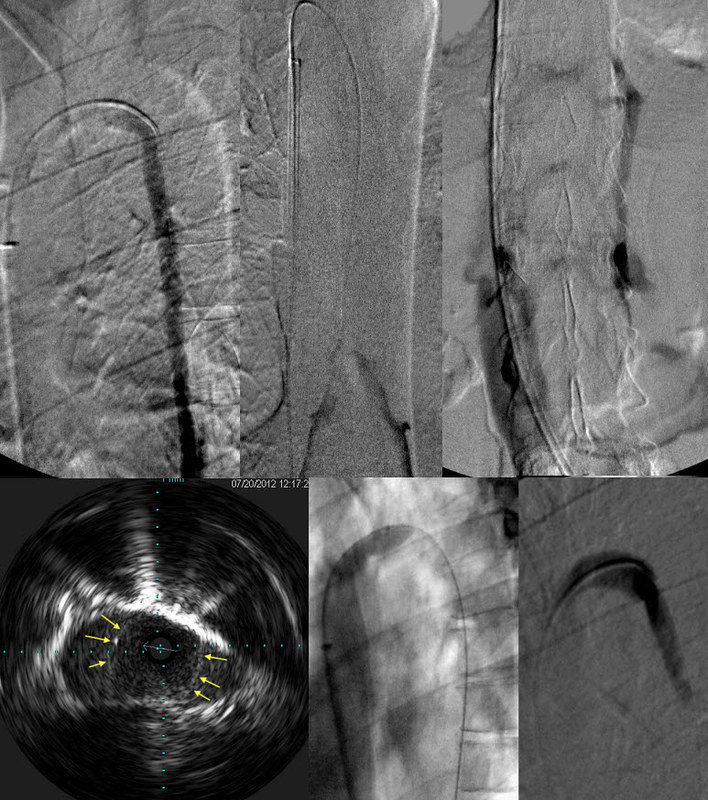
This sequence of images is quite clear.Next left internal jugular and dural sinus venography were performed.
Examination of the stents by contrast study of the dural sinus (image 2,3) showed that there was narrowing and irregularity of the contrast column as it traversed the stent.
IVUS (image 4) shows that there is in-stent thickening. The outer green line outlines the stent. The blue line outlines the stent flow (represented in red). Balloon angioplasty (image5) was performed. There was improved flow although some stenosis remains. Note that the contrast column is now smooth, fills the stent with no irregularities, only a focal stenosis. This corresponds to the narrowed stent, presumably caused by bony compression.
It seemed to respond nicely to the ballooning. If it hadn't responded well, would you have put a stent within the stent?
- drsclafani
- Family Elder
- Posts: 3182
- Joined: Fri Mar 12, 2010 3:00 pm
- Location: Brooklyn, New York
- Contact:
Re: DrSclafani answers some questions
1. most europeans are not using high pressure balloons. About half the physicians in US are using high pressure balloons. I use highest pressure balloons for all cases. Average pressure used was 13.7 atmospheres, range 8 atm to 30 atmCece wrote:
1. How common is the use of high pressure balloons? I remember you doing a survey of other IRs back around SIR or ISNVD time, was that one of the questions asked?
2. My own first procedure was about as quick as a procedure could be and that was an hour and fifteen minutes, with IVUS. Thirty minutes does not seem possible, especially considering that IVUS adds time to the procedure.
3. Is pregnancy known to contribute to restenosis in any other venous diseases?
4. When there is external compression of a stent by bone, will it continue to worsen over time, or can it be expected to be stable at the degree of narrowing that it is at?
(great image, it's striking how high the stents are, and the narrowing in the orange circle is concerning and easy to see)
5. wow, it didn't change the septum at all
2. i didnt remember your procedure being that quick. i am surprised.
3. i am not aware of such a deleterious effect. I am also not sure that she restenosed. Possible explanation may have something to do with greater blood flow during pregnancy. perhaps it did something. otherwise, i have to wonder whether it was a red herring
4. i would think that the compression is dynamic depending upon the position of the neck and head. I would not expect the compression to worsen
5. Yes, sadly, i have seen this before. I usually do not get such a beautiful longitudinal reconstructed image so this was quite graphic. I am going to focus on recreating this image in the future. I think that the septum is not likely to be successfully treated in most cases. FOr a while i tried higher pressures and larger balloons. But recently doing that did not disrupt the septum, but rather dissected the wall with the septum. and I had to stent. I will keep an eye on that case because this might become another indication for primary stenting in the future.
Salvatore JA Sclafani MD
Patient contact: ccsviliberation@gmail.com
Patient contact: ccsviliberation@gmail.com
- drsclafani
- Family Elder
- Posts: 3182
- Joined: Fri Mar 12, 2010 3:00 pm
- Location: Brooklyn, New York
- Contact:
Re: DrSclafani answers some questions
you would not be alone in thatCece wrote:In the first image, it could be mistaken for a healthy vein because the width looks good. The shade of contrast in the septum is lighter but subtle. In the second image it is clear from your labeling how narrow the opening gets but if you had shown us the image out of context, I would not have known what we were seeing.The outpocketing of contrast media to the left of the internal jugular vein represents contrast extending into the septum. To prove it I placed a catheter into the orifice of this septum (orange arrow). After balloon angioplasty the contrast column is smoother and the flow was faster but the bulge has changed little.
This is very subtle. I think that IVUS was a great teacher for things like this
Salvatore JA Sclafani MD
Patient contact: ccsviliberation@gmail.com
Patient contact: ccsviliberation@gmail.com
- drsclafani
- Family Elder
- Posts: 3182
- Joined: Fri Mar 12, 2010 3:00 pm
- Location: Brooklyn, New York
- Contact:
Re: DrSclafani answers some questions
yes, cece. And I still wonder whether there was justification to primariliy re-stent this. But how much metal is enough. Stents also add to costs and i try hard to limit the expenses to my patient. Afterall, she did need two renal stents.Cece wrote:This sequence of images is quite clear.Next left internal jugular and dural sinus venography were performed.
Examination of the stents by contrast study of the dural sinus (image 2,3) showed that there was narrowing and irregularity of the contrast column as it traversed the stent.
IVUS (image 4) shows that there is in-stent thickening. The outer green line outlines the stent. The blue line outlines the stent flow (represented in red). Balloon angioplasty (image5) was performed. There was improved flow although some stenosis remains. Note that the contrast column is now smooth, fills the stent with no irregularities, only a focal stenosis. This corresponds to the narrowed stent, presumably caused by bony compression.
It seemed to respond nicely to the ballooning. If it hadn't responded well, would you have put a stent within the stent?
Salvatore JA Sclafani MD
Patient contact: ccsviliberation@gmail.com
Patient contact: ccsviliberation@gmail.com
Re: DrSclafani answers some questions
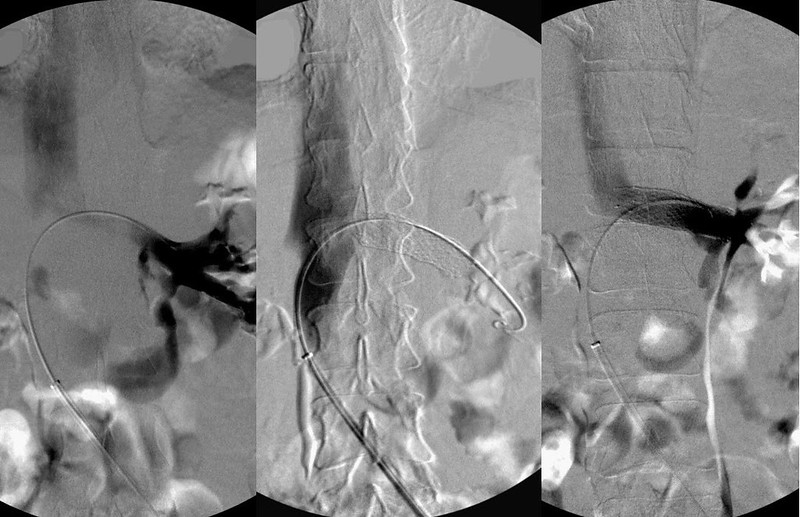
Another nice sequence of images. I especially like that the reflux into the small veins of the intervertebral plexus was captured.The azygous vein was also abnormal.
TOP ROW
With the catheter injection at the junction of the azygous arch and the ascending azygous vein, one sees NO flow of contrast reaching the superior vena cava; rather there is only retrograde flow down into the abdomen. .
The second image shows a contrast injection of the peripheral ascending azygous vein. There is reflux from confluens of azygous and hemiazygous veins with NO contrast flowing toward the superior venacava.
Finally, the third image shows reflux into the intervertebral plexus and the inferior vena cava.
OUT FLOW obstruction of the azygous vein is a problem here.
BOTTOM ROW
IVUS finds the lesion; an incomplete immobile valve in the arch of the azygous vein. (arrows outline the immobile valve). This was treated by angioplasty (middle). The resulting flow was strong and no reflux was seen. (right)
From the IVUS image, it looks like a 50% reduction in vein size. It looks like there is an opening in the middle through which flow could go, so why was there no flow at all going past that stenosis?
Re: DrSclafani answers some questions
An inflow vein of the cerebrospinal venous bed, when the cerebrospinal venous bed has enough flow and outflow obstructions of its own.
Nutcracker phenomenon results from compression of the left renal vein between the abdominal aorta and the superior mesenteric vein. The Left renal vein flows at about 550 ml/minute, which is 2-3 times the flow of both azygous and ascending lumbar veins combined. With outflow obstructions of the azygous and the ascending lumbar vein outflow, one can readily recognize the consequences of the renal vein obstruction as it converts the renal vein into an inflow vein of the cerebrospinal venous bed.
Treatment of this compressive obstruction is stenting. (image 3). Angioplasty alone is ineffective in reversing the renal vein compression.
It's so easily treated, too.