We have not had a case study in quite some time. This one was very interesting to me
The patient was a 37 year old woman with RRMS diagnosed in 2000. Symptoms at current time include fatigue, heat intolerance, head and neck pain, imbalance, numbness in both hands, weakness in both arms and legs with spasticity and requiring a wheelchair for long distance ambulation, urinary retention and constipation. She also complained of abdominal pain for many years. She had undergone extensive workup and diagnostic testing, including endoscopies, and imaging. She did not have any blood in the urine or history of kidney stones. It was thought by her neurologist that the pain might be caused by MS. Physical signs included spastic paresis of both upper and lower extremities, loss of vibratory sense in both feet, imbalance and cranial nerve deficits.
She had undergone treatment of CCSVI in 2011 at another institution which included angioplasty of both internal jugular veins with 10 mm and 12 mm balloons. She had symptomatic improvements that lasted for five months; then all symptoms came back and some were worse than before.
I thought that 12 mm balloons had been a bit small for both jugular veins. In my experience 14 mm is the average and 8mm to 26 mm is the range of balloons. Evaluation of the left renal vein, the left iliac vein and the left ascending lumbar vein were not imaged. IVUS was not used.
It seemed quite possible that inadequate treatment had been performed. I agreed to re-image and treat the patient.
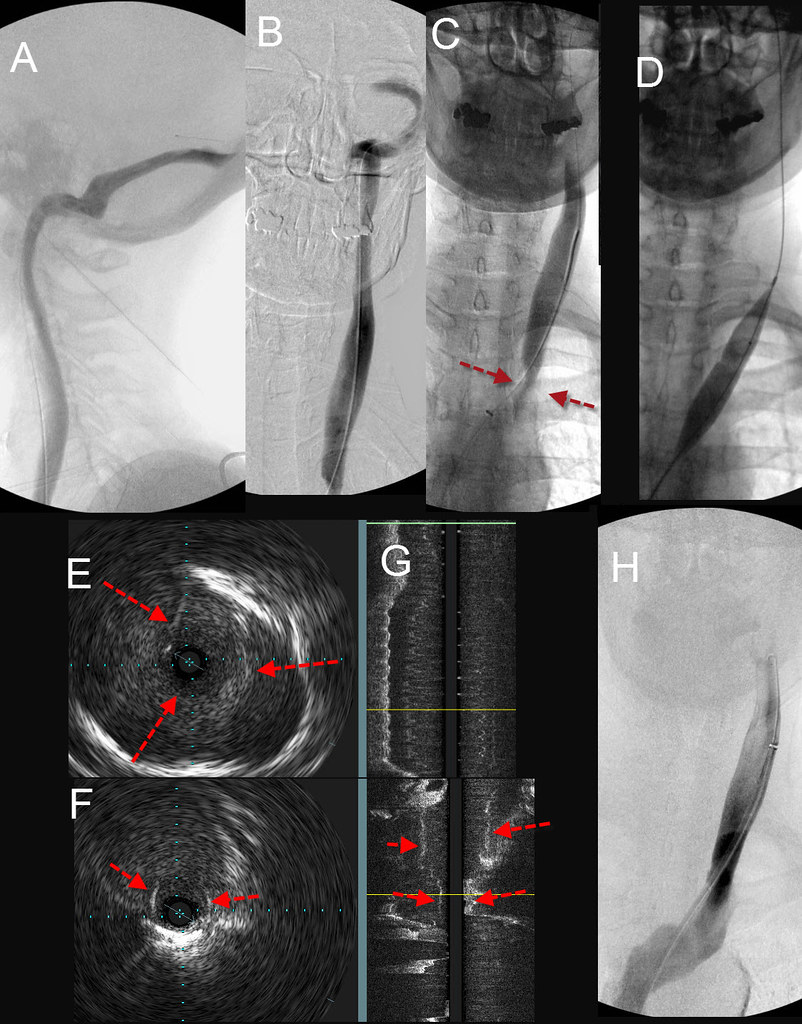
The right internal jugular study was as follows:

The first two images (top row left) show the dural sinuses. There is reflux from the right transverse sinus into the left transverse sinus and then on into the left internal jugular vein. There seem to be stenoses of both internal jugular veins at the clavicles. The next four images in the top coolumn show evidence of high grade stenosis of the valvular segment with reflux under the valve into the valve sinus.
In the lower row first two images on left IVUS is shown. There is incomplete opening of a thickened valve. The IVUS on the right outlines the valve opening and compares it to the vein area itself. The numbers below show that this represents a 66.5% stsenosis. The cross sectional area of the vein (the blue circle) measures 92.5 square millimeters. A balloon of 12 millimeter diameter has a cross sectional area of 113 square millimeters. This balloon will barely stretch the vein at the area of the valve. Any of you who have seen the bulging neck veins of a weightlifter knows how much a vein can distend under normal circumstances. My general practice is to distend the vein to about 150% of its measured cross sectional area. In this case, that would be a 14 mm balloon (csa = 150 square millimeters)
The two images on the right show the constriction of the stenotic valve during balloon inflation and the venogram after angioplasty.
LEFT INTERNAL JUGULAR VEIN
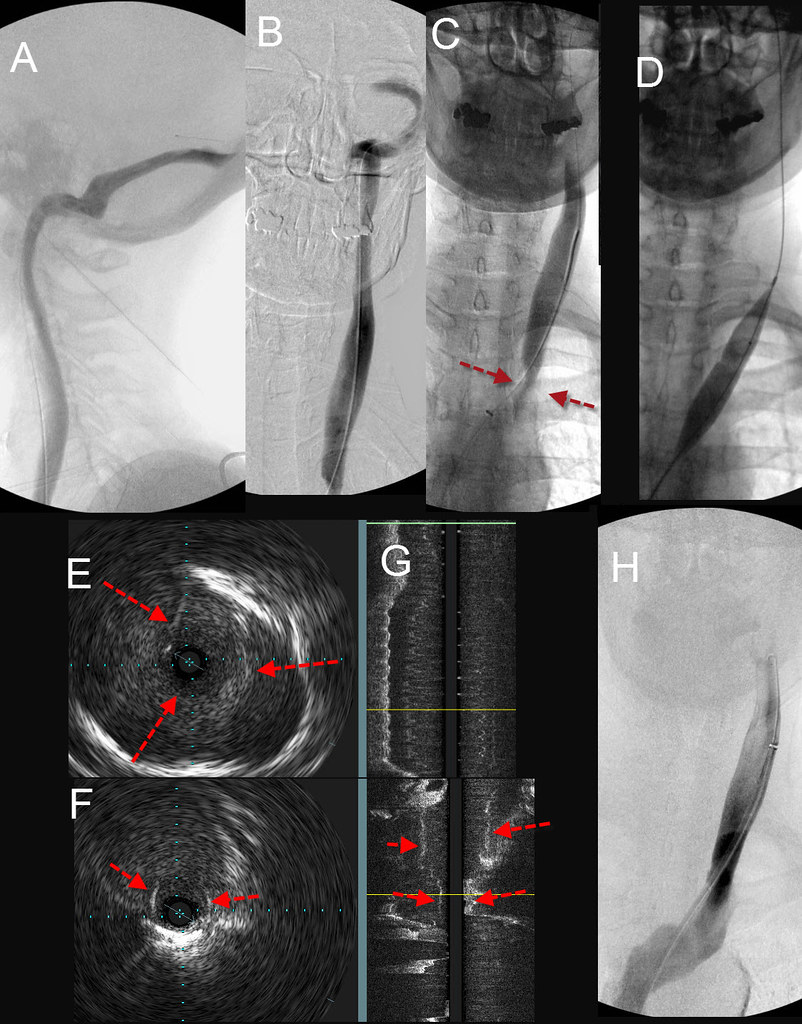
A&B show the dural sinuses. There is no reflux. However at the bottom of B, there is a suggestion of narrowing. A selective study lower down in C clearly shows a significant stenosis (red arrows). The IVUS cross sectional views (E&F) and the composite coronal image (G) show thickened tissue that may represent a valve or a septum dividing the vein into two channels. While not shows, the cross sectional area of the vein in E measured about 160 square millimeters. Based upon my 150% balloon size algorithm, a balloon of about 250 square millimeters is necessary. That equates to an 18-millimeter diameter balloon. (figure D). After angioplasty (H) the vein diameter is much improved and flow was faster.
We have discussed many times how it is common to underestimate balloon size without IVUS and I am not showing this case for that reason. Rather I thought that the most interesting component was the renal vein imaging.
LEFT RENAL VEIN

The image on the left (A) is the venogram of vein of the left kidney. The darkness (density) of the contrast media is less in the circled area where the vein crosses between the aorta and the superior mesenteric artery as can be seen in Image C. The narrowed cross sectional area (in green on figure D) represents the renal vein at the area of narrowing. In Image D you can see that the vein is compressed between the SMA and the aorta. On the longitudinal vein (Image E) the narrowing in Green clearly indicates the stenosis. The calculations in image D show that this stenosis is greater that 95%. Images F and G faintly show the outline of the stents.
So why do I show this case? We have seen renal vein compressions in many other case studies. My recent analysis has shown that the incidence of renal vein compression stenosis is much more common and the degree of stenosis are much more severe in patients with MS when compared to healthy controls.
The patient's clinical symptoms included severe abdominal pain that was relieved only by lying down. She has underdone multiple endoscopies without detecting any abnormalities. In the absence of objective findings, some believed that the inflammatory brain and spine disease was the cause of it.
I will now quote the patient's subjective results of stenting:
patient response five days after treatment wrote:I hope this email finds you well. I wanted to give an update on my situation, but before I do I wanted to reiterate how thankful I am for all that you have performed on me and on so many others. Again, thank you.
My parents and I left Brooklyn Saturday at 11:00 and drove back home. We stop every two hours of less so that I could stretch my leg and walk. I tried to walk as much as I could but the pain was very intense (pain from the stents in my back).
Since my intervention last Friday, I have notice improvements. My vertigo is almost gone, my balance is better, my foot drop is less, my bladder works better, so far no headaches, but the most amazing improvement is that my stomach pain is gone! I wasn't expecting for that and that was the worse of all of my issues. I can now eat without having to lie down immediately after, I am able to live in a more normal way. This is simply incredible!
The back pain from the stents is very slowly diminishing. I only take Tylenol.
Nutcracker syndrome, like CCSVI, is another entity that is not universally accepted as a clinical problem. Some say that it occurs in healthy patients. However it does cause pain and that pain may resolve after relieving the obstruction. This is not the first patienet who had pain relieved by stenting. In one patient that patient just expected to live with this pain, having never spoken to her doctor about it. This pain is often ascribed to ovarian pain, ovulation, muscle strain, and now even MS. I think that occlut abdominal pain without an explanation should be evaluated for nutcracker because of the high incidence. If one is not undergoing venography for ccsvi diagnosis and treatment, MRI or CT venography of the abdomen can pinpoint the compression. Venography is considered the Gold Standard for diagnosis but I believe that IVUS is by far superior to venography in assessing this compression stenosis.
Any questions?