We have previously spoken about the scenario of this week's case of the week: A procedure totally done using IVUS for diagnosis and intervention. Venography was not performed.
The patient is a 53 year old female who has symptoms resembling MS, including severe confusion, difficulties in multi-tasking, with severe short term memory loss and profound fatigue. She also has weakness without spasticity, incoordination and lack of balance. Her doctors have yet to give her a diagnosis of MS despite evidence of demyelination and progressive deterioration.
The patient and her husband traveled to Bangalore, India in 2010 to have venography and venoplasty. During that visit external Doppler ultrasound of the neck vessels was performed. It was said to show CCSVI; however the examination was done looking at velocities and flow and used the Valsalva maneuver. It showed reflux.
Venography was then attempted. The procedure was begun by right femoral access. The patient states that she recalls that one of the vessels was catheterized and that she heard the doctors note that there was a stenosis. However, she does not know which vessel was referenced. The next few minutes became unclear to the patient and she developed anaphylactic shock requiring resuscitation. Resuscitation was successful but the procedure was terminated. The patient returned to Canada, alive, knowing that there was some stenosis but untreated.
She and her husband persisted., seeking a way to undergo another attempt, but obviously unable to have standard venography or venographic guidance to treatment. They tried MR venography. There is no cross reactivity between venographic dye and MR dye. They are separate, different compounds with nothing in common. There is no association of allergic reactions between the two. Nonetheless she had an allergic reaction. They were investigating the use of carbon dioxide gas as a contrast agent, something researched extensively by Irwin Hawkins and Jim Caridi in Florida.
At the same time, i reached out to patients who had not been given followup to their inquiries back in the days when i started treatment at American Access. I emailed many patients expressing my regret that timely follow-up had not been done and to inform them that things had finally been ironed out. And that is how I became involved in this patient.
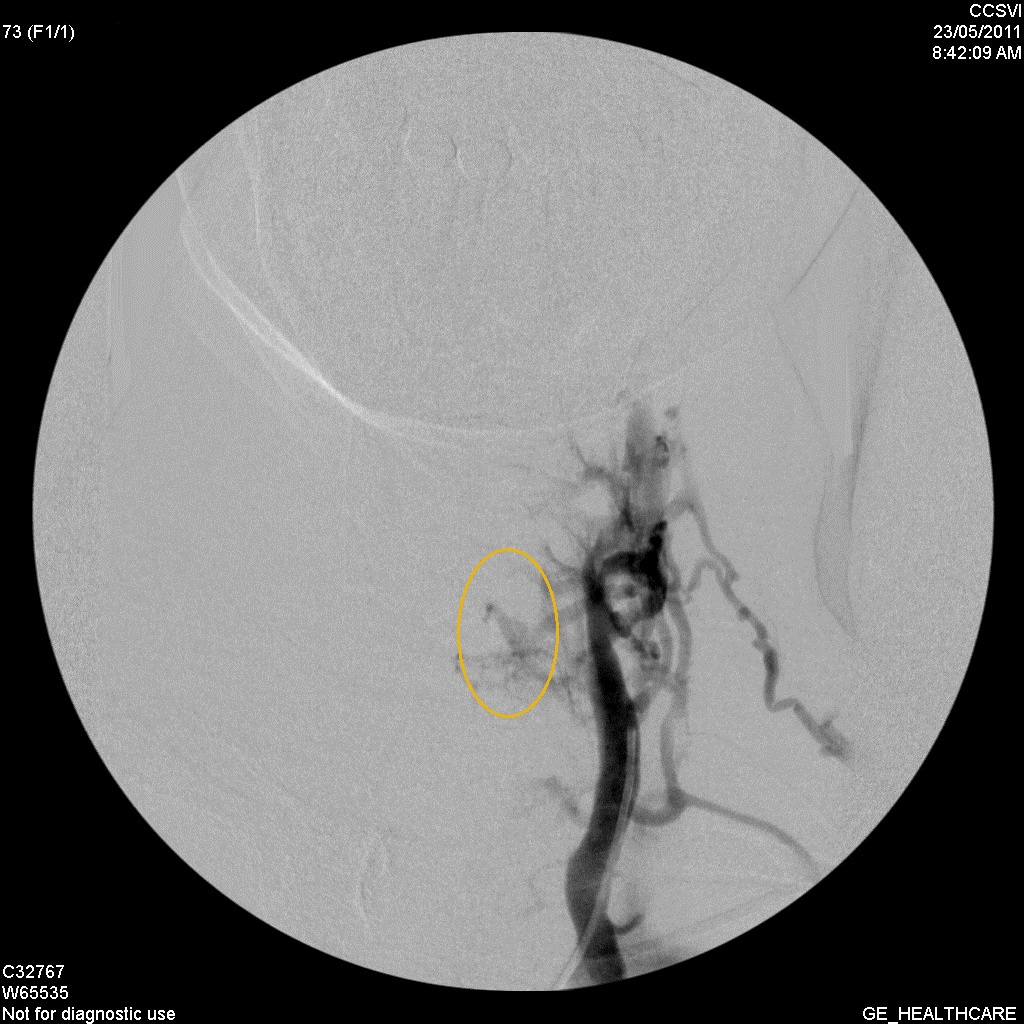
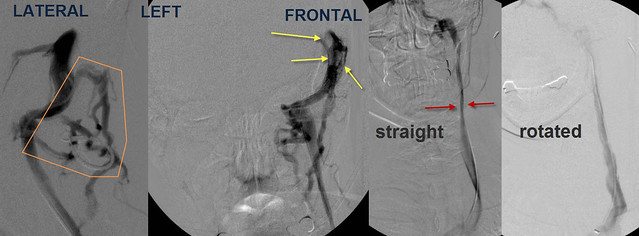
I told her that I would be willing to attempt the procedure without the use of any dyes and use fluoroscopy and IVUS for guidance, diagnosis and treatment. Fluoroscopy would give me landmarks. The bones visible on fluoroscopy would enable me to know where the trouble was. Finding the trouble would require the use of IVUS to show me stenoses and valvular abnormalities.
Catheterization began from the left saphenous vein just before it entered the femoral vein. The sheath was placed in the superior vena cava thus avoiding any further instrument placement through the heart. At this time i then administered intravenously benadryl, an antihistamine which promptly caused the heart rate to rise to greater than 160 beats/minute. This was treated and the pulse returned to 80 ppm. Blood sugar had dropped to 53 so 50% dextrose was given. Finally things returned to her steady state and we resumed the procedure.
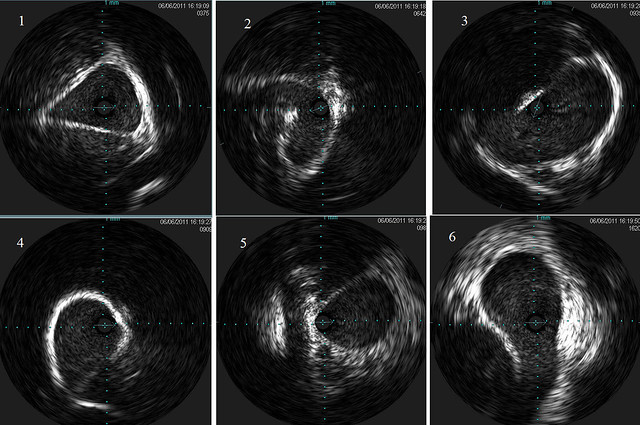
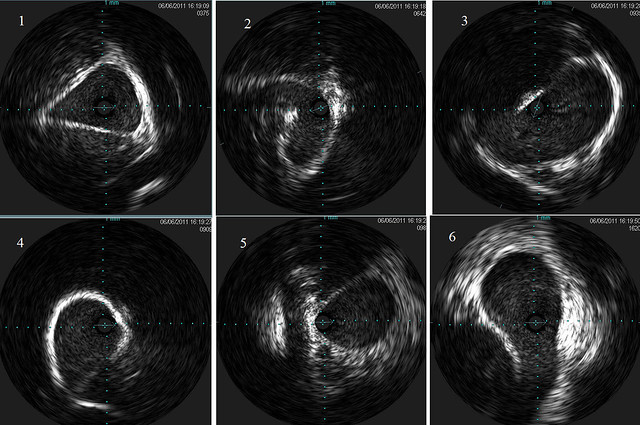
Selective catheterization of the right internal jugular vein was performed first. I knew i was in the jugular vein because of the guidewire went into the dural sinuses. I exchanged the catheter for the IVUS device which i advanced into the dural sinus. I created IVUS images as i pulled the device through the dural sinus, the bony jugular bulb and finally through the jugular vein into the inominate vein. See the twelve IVUS images that make up the right jugular vein.
and

[/img]
I will be back later to answer some questions and to review this part of a very interesting case.




 [/img]
[/img]