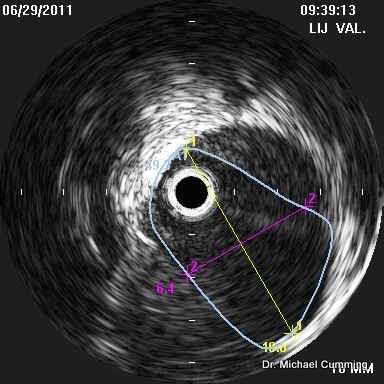
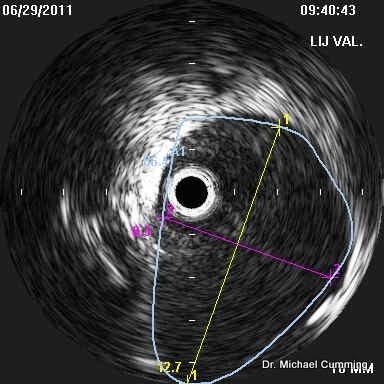
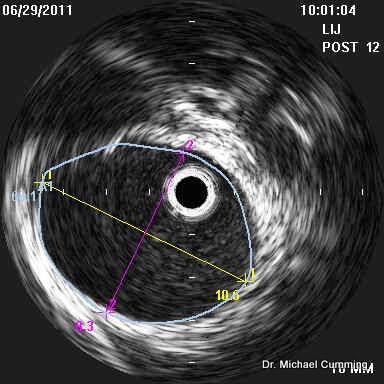
Firstly, in PwMS, surface B-mode and Doppler ultrasound almost always shows hemodynamic derangements when performed by the zamboni protocol and performed and interpreted by someone qualified to do so by training.CureOrBust wrote:I was obviously not clear enopugh, my question was if these issues were not visible under fluoroscope, would they present themselves as flow issue under a standard CCSVI doppler; errr... by standard I guess we would have to take Zamboni's measures...drsclafani wrote:Perhaps it is just me, but i find that the majority of azygous valvular abnormalities are not visible on venography but visible on IVUS.CureOrBust wrote:I understand this question may be a bit much to ask at this early stage, but roughly, or if at all, what percentage chance do you think would there be of someone not showing issues on a standard external Doppler and no issues in a venography, but IVUS would find something? from a purely diagnosis perspective.
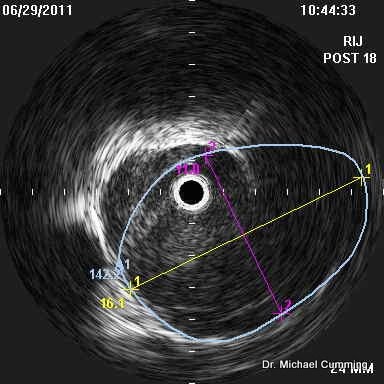
But IVUS is not just about making a diagnosis. it is also about a treatment plan, balloon sizes, and assessment of the effects of angioplasty. It can also detect dissections after angioplasty that may go unrecognized without ivus.
Secondly, these ultrasound abnormalities reflect problems with the global hemodynamics of the cerebrospinal venous circults
thirdly, they do not usually reflect some particular pathologic site of stenosis
Thus ultrasound is extremely sensitive to deranged hemodynamics but is n ot specific as to the veins that are problematic.
Ultrasound can rarely be used to pinpoint problems in the azygous vein.
Secondly