I will admit that, after you revealed yourself, I went back to reread your earlier post to Dr. Sclafani about your wife's fatigue and balance improvements. That's the stuff we don't always hear about at the end of one of Dr. Sclafani's cases. He opens the veins as best he can but after that it's out of his hands. There has to be something that will predict improvements but they haven't found it yet that I know of.MikeInFlorida wrote:Thank you for pointing that out. I thought I had given away the surprise ending.Cece wrote:He mentioned this here too.
My wife has always been an overachiever. Even with diseases.Cece wrote:At the least, this case gave Dr. Sclafani a workout. And we like to see him challenged.
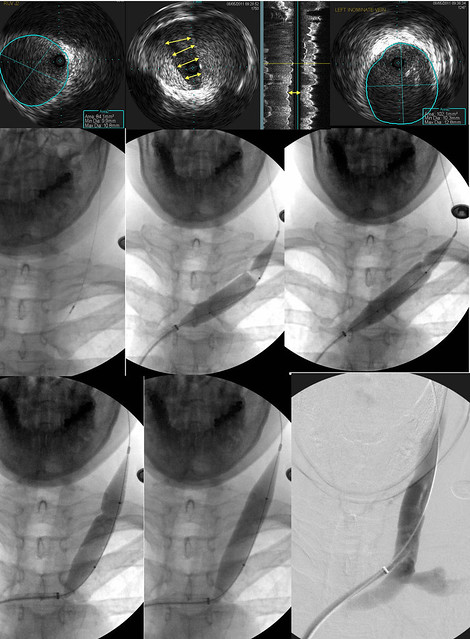
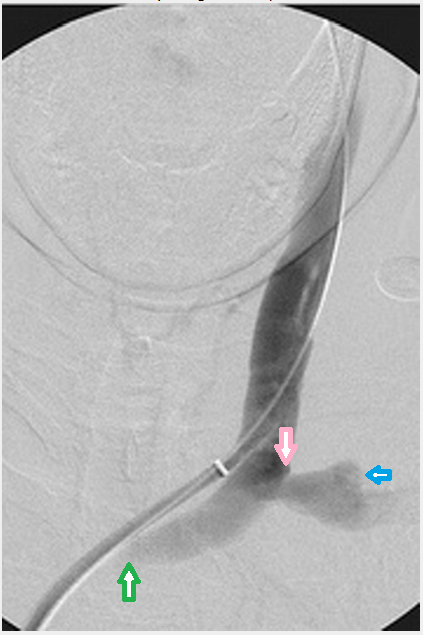
My thought now is that the stenosis in the innominate is causing the flow entering from the jugular to reflux back into the subclavian. Thus the puff. The flow from the jugular is looking for another way out when it hits the innominate stenosis. It does not have to be a full occlusion, only a partial one, to cause reflux.I feel free to comment here, since I am in the dark on what this picture means. I think I agree with you, Cece, that this is the subclavian... it looks like the correct geography. But why would it reflux in that direction? The innominate must have an opening (even with a stenosis), or the IJV could not have been accessed. If there is an opening, there should be flow. If there is flow, the contrast should be pushed into the SVC.Cece wrote:Dr. Sclafani, would the 'puff' of contrast out to the side be the contrast refluxing into the subclavian?
If the flow from the subclavian were stronger, it might prevent reflux in this direction, but the subclavian has a stenosis of its own.