mtf wrote:Hi Dr.,
Thanks alot for your help last week. I'm happy that my left lgv isn't trombosed but now I have other to think about (occlusion/trombos) near my brain. Can you please, now, tell me what do you think about my veins?
Thank you very much (it was very good to talk to you) .
Dear MTF,
it was a pleasure to meet you in Lisboa.
for the group's curiosity, I was visiting MTF's doctor to learn from him a new treatment for enlarged prostate glands that result in difficulties with urination. In that treatment a very tiny catheter is placed into the arteries that supply oxygenated blood to the prostate gland. Fine particles are injected to block these arteries and this results in the ability to urinate without drugs that may make men impotent. It is a challenging procedure and I admire MTF's doctor for the skill and dedication he shared with me.
As it turned out, MTF and another patient with MS came to visit him that day, perhaps because i was visiting and I watched advised her doctors as they repeated the procedure.
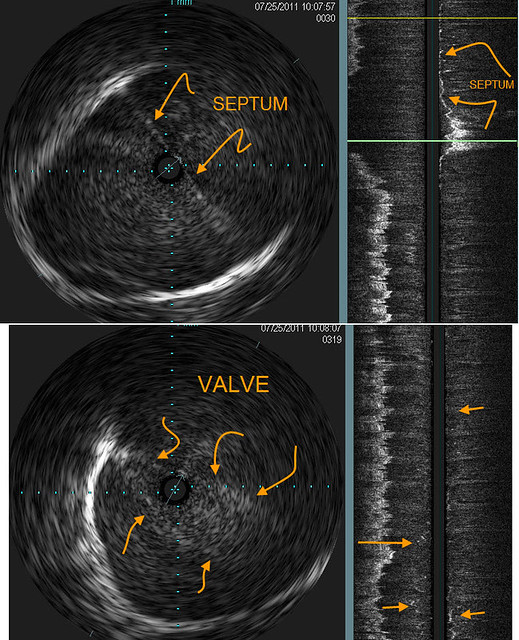
I gave them some critical pointers that led to the change of diagnoses from occlusion of the J1 segment of the left IJV to in-stent stenosis of both internal jugular veins. These were treated with angioplasty. I also advised that they look at the upper part jugular veins that had not been looked at before. Regretably, this showed that there seemed to be obstructions higher up in the jugular veins that had not been previously recognized. I say "seemed to be" because they were unable to advance the guidewire or the catheter into the dural sinuses and thus could not confirm continuity between the dural sinus and the jugular vein. so it was not definite but highly probable. It is possible for improvement of flow by opening the lower stenoses even with an upper obstruction.
Perhaps, mtf, it would be useful to have an MRV to look for continuity or lack of continuity. However MRV can sometimes be misleading in this regard.
If there is no continuity between the jugular and the dural sinus, there is nothing I can think of to relieve that situation. It is too high for bypass.
Most importantly, how are you feeling? I admire your bravery and leadership. Dr P seems to feel the same way.
Best
DrS