Rosegirl wrote:Dear Dr. Sclafani,
Dr. Zamboni and others cautioned patients to wait for proven protocols if their condition warranted it. No major trials have been completed yet, but, based on your experience, can you give an overview of what is most likely to improve?
This is a wise and politically appropriate caution. However some patients choose to have a procedure done before completion of trials because there are difficulties in getting trials started and finished. Moreover, doing trials without first analyzing safety and best practice made no sense either. So as I have no funding to do a trial, I continue to treat patients based on compassionate grounds, my own assessment of the validity of treatment and my own sense of risk/benefit analysis. Had outcomes of treatment been worse or risks more profound, I likely would have stopped treating as risk/benefit trumps compassionate use in my ethics.
That said, I have now learned many things
1. I cannot predict who will get benefits
2. I cannot set the value of benefits to an individual
3. The risks are now very low
4. my protocol is set
5. I do not have clarity regarding compression narrowings of the J2 segment, nor a good IR treatment of J3 impingements. Need more data before stenting them.
6. I do not want to stent the internal jugular veins except for bale out of complications or possibly stenoses persistently resistent to angioplasty
7. The evaluation of the Nutcracker syndrome is absolutely essential in patients with MS.
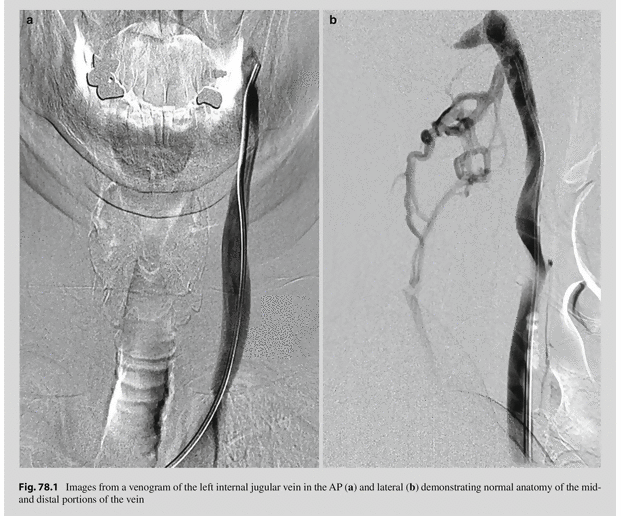
8. IVUS is very important for diagnosis and treatment planning, and assessment of angioplasty outcomes
9. Large high pressure balloons are essential
10. Primary progressive MS is different. While some patients do get improvements, many do not
11. I have seen every disability improved in at least one patient
12. most common improvements seem to be brainstem functions, such as cranial nerve function (diplopia, visual disturbance, dysarthria and dysphonia, swallowing difficulties) sympathetic nervous function (sweating, bladder difficulties, etc), temperature regulation, fatigue, balance. Other common improvements include relief from cognitive impairment, memory, fatigue, depression
13. severe ataxia rarely resolves, but may improve
14.
15. Improvements can take up to a year to be manifest. (One patient with hypothalamic dysfunction manifested in spermatogenisis took over one year to return to normal.)
16. A poor start on research, a fascination with replicating Zamboni's work on ultrasound, and a general, out of proportion, negativity to the concepts regarding the role of ccsvi as a cause of MS rather than as a method of symptom relief have distracted from good research partnerships.
For those who have trouble walking, it seemed that the patient either got complete relief or no improvement at all.
walking disability is complicated because spastic paralysis and paresis, imbalance, and fixed foot drop, together with a generally unfit physique impair ability to improve walking in many patients. Improvements in ambulation often take a very long time but do occur. Unfortunately dead neurons cannot be resurrected. However dysfunctional neurons can be made to work better in my belief.
And for those non-responders or patients who relapsed after treatment, is there a limit on how many times and how often one might have a CCSVI procedure?
first, patients who have return of disability:
1. early relapse of definite improvements suggests thrombosis or restenosis of treated veins. Venography should be repeated.
2. If this were an insured treatment, I would recommend follow-up venography in three months routinely regardless of .
3. If I suspected thrombosis, I would urgently perform ultrasound and if thrombosis was confirmed I would rush to venography and restore flow asap
4. No restenosis or thrombosis is found on followup venography and the initial examination performed was detailed, included IVUS, and imaged the dural sinuses, both jugular veins and brachiocephalic veins, the azygos vein, the left renal vein, the left iliac vein, I would suspect a placebo effect that dissipated.
Similarly for 'nonresponders:
1.if the exam was detailed, included IVUS and all relevant veins, I would think that neuonal death has trumped CCSVI flow deficits and that the treatment will not work.
2. if the exam was not a complete one, I would have no hesitation to repeat it as some patients with incomplete treatments can get better by doing the full deal. Witness Marcus' (Pukai's) improvements that really got better only after treatment of the nutcracker syndrome's contribution to spinal cord venous congestion.